Recurrent Implantation Failure (RIF) is hard to deal with and can be very discouraging for couples going through IVF failure or other fertility methods. It happens when transferring more than one egg does not lead to a baby. This piece will talk about what causes recurrent implantation failure, diagnosis and treatment, systematic review, and meta-analysis to get past it. It will give people who are trying to get pregnant hope and direction.
What does “Recurrent Implantation Failure” Mean?
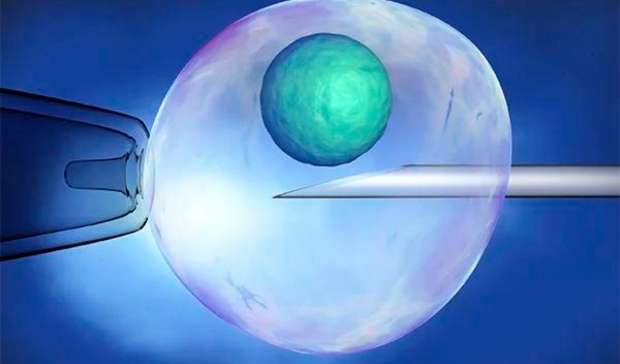
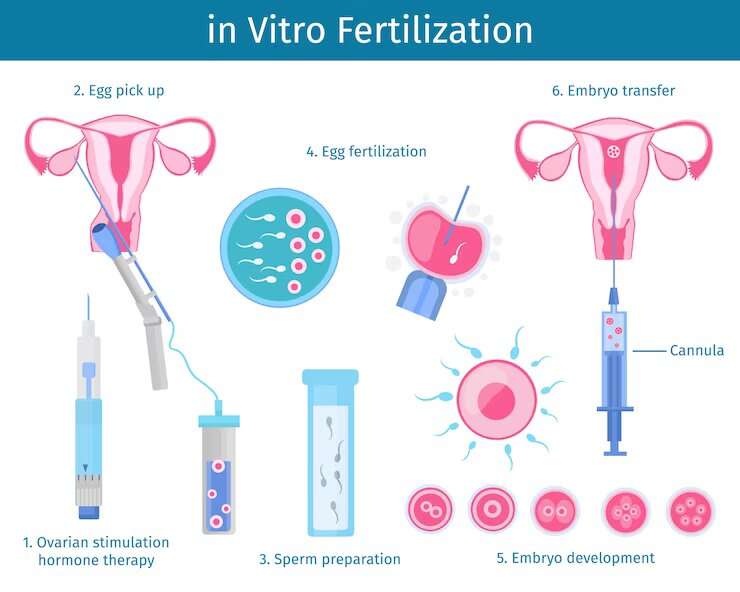
When at least three high-quality embryos have been transferred during repeated IVF cycle rounds and a clinical pregnancy rate has not been achieved, this is called recurrent implantation failure after in vitro. RIF patients who want to have a child may find this situation hard on their minds and bodies.
Causes of Recurrent Implantation Failure
Women with recurrent implantation failure have a low implantation success rate, and finding the root reasons is important for successful implantation.
Endometriosis: Recurrent miscarriage can make the uterus environment worse, which can make it harder for a baby to implant. Taking care of your endometriosis before you try IVF might increase your chances of success.
Uterine Abnormalities: Problems with the structure of the uterus, like tumors or polyps, can make it hard for the baby to grow. Some of these problems might need to be fixed with treatment options like surgery
Immune System Effects: If the immune system reacts too strongly, it may reject embryos. Therapies that change the immune system can be thought about.
Genetic Problems: The genetic makeup of both partners can affect the survival of the baby. Preimplantation genetic testing, or PGT, can improve implantation and pregnancy rates.
Thrombophilia: Women with recurrent problems with blood clotting can make it hard for blood to get to the uterus, which can make it hard for the baby to grow. People may receive blood-thinning medications.
Treatment for Repeat Implantation Failure
The treatment approach for RIF depends on its underlying cause. These are some common plans for patients with recurrent implantation failure:
Making changes to your lifestyle: Living a healthy life with a balanced diet, regular exercise, and less stress can decrease your fertilization failure.
Endometrial Receptivity Analysis (ERA): This test checks the lining of the uterus to find the best time to move the egg, which increases the chances of treatment of recurrent
Hormonal Therapy: Treatments based on hormones can make the uterus more open, keep the period regular, and lower immune responses.
Surgical Interventions: Fixing problems with the uterus through surgery, like hysteroscopy or myomectomy, can raise the chances of implantation.
Immunomodulation: To keep the baby from being rejected, the immune system may need to be slowed down or changed.
Genetic Screening: PGT can find embryos that have problems with their genes, making sure that only healthy embryos are transferred.
Thrombophilia Management: If thrombophilia is a problem, medicines that thin the blood may be given.
Success After Several Failed Embryo Implantations
Embryo Implantation Failure does not mean you can’t have children. After dealing with the root reasons, many patients with rif can have healthy babies. It’s important to work closely with a fertility expert who can make a treatment plan just for you.
Conclusion
Unexplained Recurrent Failure after in vitro fertilization is a tough problem that can be solved on the way to having a child. Many couples can get over this problem and finally have the child they want if they fully understand what causes it and what treatments are available. If you’re dealing with RIF, talk to a fertility expert. They can help you through your journey and give you personalized care.
FAQs Regarding Implantation Failure Patients
1. What is the success rate of patients with repeated implantation failures?
RIF doesn’t happen very often; only 5–10% of couples going through IVF get it. The frequency may change based on the person’s situation and the root reasons.
2. Can I make changes to my habits that will help stop repeated unexplained implantation failure?
Adopting a healthy lifestyle that includes a well-balanced diet, regular exercise, and ways to deal with stress can help with fertility and lower the risk of RIF.
3. How many IVF attempts do you need to have before the implantation fails again?
Most of the time, recurrent implantation failure and recurrent is identified after at least three IVF rounds with healthy egg transfers that don’t lead to a baby.
4. Is it possible to treat women with repeated implantation failure?
Of course, many couples with RIF can have healthy babies after getting the right evaluation and care.
5. How does mental support role in implantation failure in IVF?
During RIF treatment, mental support is very important because the process can be hard on the emotions. Fertility treatments can be stressful, but support groups, counseling, and being honest with your partner can help.






 :
:

