प्रेगनेंट नहीं होने के कारण आजकल कई दंपतियों के लिए चिंता का विषय बन गए हैं। अगर आप लगातार प्रयासों के बाद भी गर्भधारण (कंसीव) नहीं कर पा रही हैं, तो सबसे पहले यह समझें कि आप अकेली नहीं हैं – विश्व स्तर पर हर 6 में से 1 व्यक्ति को गर्भधारण की समस्या का सामना करना पड़ता है। महिलाओं में बांझपन हो या पुरुषों में, इसके पीछे मेडिकल, हार्मोनल और जीवनशैली से जुड़े कई कारण हो सकते हैं। अच्छी खबर यह है कि प्रेगनेंट नहीं होने का इलाज आज आधुनिक चिकित्सा के जरिये संभव है और ज्यादातर मामलों में सही मार्गदर्शन व उपचार से संतान का सुख पाया जा सकता है। इस विस्तृत लेख में हम प्रेगनेंट नहीं होने के सभी संभावित कारणों पर चर्चा करेंगे और साथ ही प्रभावी इलाज, घरेलू उपाय, जीवनशैली में बदलाव, भावनात्मक पहलू और आधुनिक तकनीकों (IUI, IVF आदि) के बारे में जानकारी देंगे। यदि आप गर्भधारण की समस्या से जूझ रहे हैं तो यह लेख आपके लिए है, जिससे आप अपने माता-पिता बनने के सपने को साकार करने के रास्ते खोज सकें।
महिलाओं में प्रेगनेंट नहीं होने के कारण (महिलाओं में बांझपन)
महिलाओं में बांझपन (Female Infertility) के पीछे कई मेडिकल और हार्मोनल कारण हो सकते हैं। अक्सर समस्या महिला की प्रजनन प्रणाली से संबंधित होती है – जैसे अंडाशय में अंडाणु बनने या निकलने में परेशानी, अंडों का गुणवत्ता संबंधी मसला, या प्रजनन अंगों में रुकावट। आइए महिलाओं में प्रेगनेंट नहीं होने के कारण को बिंदुवार समझें:
- ओव्यूलेशन संबंधी विकार: अनियमित या न होने वाला ओव्यूलेशन (अंडोत्सर्जन) महिलाओं में प्रेगनेंट नहीं होने का सबसे आम कारण है। उदाहरण के लिए पीसीओएस (Polycystic Ovary Syndrome) एक हार्मोनल विकार है जिसमें अंडाशय में सिस्ट बनने से हार्मोन असंतुलन हो जाता है और पीरियड्स अनियमित हो जाते हैं, जिससे अंडा समय पर रिलीज़ नहीं होता। इसके अलावा थायरॉयड हार्मोन का असंतुलन या प्रोलैक्टिन हार्मोन बढ़ना भी ओव्यूलेशन को प्रभावित करके गर्भधारण में बाधा डाल सकते हैं।
- फैलोपियन ट्यूब में अवरोध: अगर महिला की फैलोपियन नलियाँ (Fallopian tubes) बंद या क्षतिग्रस्त हों, तो शुक्राणु और अंडाणु का मिलन नहीं हो पाता। पेल्विक इन्फ्लेमेटरी डिज़ीज (PID) जैसी संक्रमण, ट्यूबरकुलोसिस, या एंडोमेट्रियोसिस के कारण ट्यूब में रुकावट आ सकती है। ऐसी स्थिति में प्राकृतिक गर्भाधान मुश्किल हो जाता है क्योंकि निषेचित अंडा गर्भाशय तक पहुंच ही नहीं पाता।
- गर्भाशय एवं गर्भग्रीवा की समस्याएँ: गर्भाशय में फाइब्रॉइड (गाठें) या पॉलिप होना, गर्भाशय के आकार में विकृति, या गर्भग्रीवा (सर्विक्स) में संक्रमण/म्यूकस की समस्या के कारण भी गर्भ ठहरने में दिक्कत आ सकती है। गर्भाशय का अंदरूनी अस्तर (एंडोमेट्रियम) स्वस्थ न होना या बहुत पतला/मोटा होना भी निषेचन को बाधित कर सकता है।
- एंडोमेट्रियोसिस: इसमें गर्भाशय की अंदरूनी परत की कोशिकाएँ गर्भाशय के बाहर फैल जाती हैं (जैसे अंडाशय, ट्यूब या पेट के अन्य अंगों पर)। एंडोमेट्रियोसिस से अक्सर तेज दर्द होता है और यह फैलोपियन ट्यूब व अंडाशय पर जलन और चिपकाव (scar) बनाकर गर्भधारण में समस्या पैदा कर सकता है।
- आयु का प्रभाव: उम्र बढ़ने के साथ स्त्री की प्रजनन क्षमता घटती है। विशेषज्ञों के अनुसार 20 से 35 वर्ष की आयु गर्भधारण के लिए आदर्श मानी जाती है। 35 के बाद अंडों की गुणवत्ता और संख्या दोनों कम होने लगती हैं, जिससे गर्भधारण की संभावना घटती है। 40 के पार ये चुनौतियाँ और बढ़ जाती हैं। हालांकि आजकल उपलब्ध इलाज की मदद से अधिक उम्र में भी मां बनना संभव है, लेकिन प्राकृतिक रूप से अवसर कम हो जाते हैं।
- अन्य चिकित्सीय स्थितियाँ: कुछ अन्य कारण जैसे गर्भाशय में पुराने संक्रमण, पेल्विक सर्जरी से बना निशान (scar tissue), प्राइमरी ओवेरियन इन्सफ़िशिएंसी (कम उम्र में ही ओवरी का काम बंद होना), ऑटोइम्यून विकार (जैसे ल्यूपस), या अनुवांशिक विकार भी महिलाओं में बांझपन का कारण बन सकते हैं। इन स्थितियों में विशेषज्ञ द्वारा विस्तृत परीक्षण की आवश्यकता होती है।
उपरोक्त कारण महिलाओं में गर्भधारण न होने के प्रमुख कारक हैं। अच्छी बात यह है कि इनमें से ज्यादातर समस्याओं का उपचार उपलब्ध है या इन्हें प्रबंधित किया जा सकता है। सही निदान के बाद डॉक्टर दवाओं, हार्मोन थेरेपी या सर्जरी द्वारा उपचार करके गर्भधारण की संभावना बढ़ा सकते हैं।
पुरुषों में गर्भधारण न होने के कारण (पुरुष बांझपन)
लगभग एक-तिहाई मामलों में गर्भधारण में समस्या पुरुष साथी की वजह से होती है। पुरुष बांझपन (Male Infertility) मुख्यतः शुक्राणुओं (स्पर्म) की संख्या, गुणवत्ता या गतिशीलता में कमी के रूप में सामने आती है। पुरुषों में प्रेगनेंट नहीं होने के कारण निम्न हो सकते हैं:
- शुक्राणुओं की संख्या या गुणवत्ता में कमी: वीर्य में स्वस्थ शुक्राणुओं की पर्याप्त संख्या का न होना (ओलिगोस्पर्मिया) या शुक्राणुओं का आकार/आकार में गड़बड़ी (टेरेटोज़ूस्पर्मिया) गर्भाधान को कठिन बना देता है। बहुत कम शुक्राणु होने पर वे अंडाणु तक पहुंच ही नहीं पाते, जिससे निषेचन नहीं हो पाता।
- शुक्राणुओं की धीमी गतिशीलता: कुछ पुरुषों के शुक्राणु पर्याप्त तेज़ी से तैर नहीं पाते या गर्भाशय तक पहुंचने से पहले ही मर जाते हैं। शुक्राणुओं की गतिशीलता (Motility) कम होने पर वे अंडे तक पहुंचकर उसे फर्टिलाइज़ नहीं कर पाते।
- वृषण (टेस्टिकल) संबंधी समस्याएँ: वृषणों में किसी चोट या संक्रमण का पुराना प्रभाव, वरीकोसील (Varicocele) यानी अंडकोष की नसों का फूलना, या बचपन में अंडकोष का सही से नीचे न उतरना (अनडिसेंडेड टेस्टिस) जैसी स्थितियाँ पुरुष प्रजनन क्षमता को कम कर देती हैं। वरीकोसील से अंडकोष का तापमान बढ़ जाता है और शुक्राणु की संख्या/गुणवत्ता घट सकती है।
- हार्मोनल असंतुलन: पुरुषों में टेस्टोस्टेरोन और एफएसएच/LH जैसे हार्मोन का असंतुलन होने पर शुक्राणु उत्पादन प्रभावित होता है। हाइपोगोनैडिज्म (Low Testosterone) की स्थिति में शरीर पर्याप्त स्वस्थ शुक्राणु नहीं बना पाता। पिट्यूटरी ग्रंथि में ट्यूमर या अन्य विकार भी हार्मोन के उत्पादन को प्रभावित कर पुरुष बांझपन पैदा कर सकते हैं।
- यौन दुर्बलताएँ: शीघ्रपतन, नपुंसकता (इरेक्टाइल डिस्फंक्शन), या शुक्राणु स्खलन संबंधी समस्याएँ (जैसे रेट्रोग्रेड एजाकुलेशन, जिसमें वीर्य बाहर निकलने की बजाय मूत्राशय में चला जाता है) से भी दंपति को गर्भधारण में कठिनाई हो सकती है। यदि पुरुष संभोग के दौरान स्वस्थ वीर्य बाहर नहीं छोड़ पाता, तो गर्भधारण संभव नहीं होगा।
- अन्य कारक: कुछ दवाओं या एनाबॉलिक स्टेरॉइड का दुरुपयोग, अति गर्मी के संपर्क (लगातार गर्म पानी के टब में बैठना, गोद में लैपटॉप रखना, बहुत टाइट अंडरवियर पहनना) से अंडकोष का तापमान बढ़ना, जिससे शुक्राणु को नुकसान होता है। पिछले कैंसर उपचार (किमोथेरेपी/रेडियोथेरेपी) या गंभीर बीमारियाँ भी पुरुष प्रजनन क्षमता घटा सकती हैं। इन्फेक्शन (जैसे以前 मम्प्स से अंडकोष में सूजन) या यौन संचारित रोगों से हुए संक्रमण के कारण शुक्राणु मार्ग अवरुद्ध होना भी एक कारण हो सकता है।
पुरुषों में कई बार बांझपन के स्पष्ट बाहरी लक्षण नहीं दिखते, इसलिए यदि गर्भधारण नहीं हो पा रहा है तो पुरुष साथी का स्पर्म एनालिसिस करवाना ज़रूरी है। अच्छी बात यह है कि पुरुष बांझपन के लिए भी अनेक उपचार उपलब्ध हैं – दवाओं से लेकर सर्जरी तक – जिनसे शुक्राणुओं की संख्या व गुणवत्ता में सुधार लाकर गर्भधारण की संभावना बढ़ाई जा सकती है।
जीवनशैली और अन्य सामान्य कारक
कुछ आम जीवनशैली से जुड़ी आदतें और स्वास्थ्य कारक भी स्त्री या पुरुष की प्रजनन क्षमता को प्रभावित कर सकते हैं। कई बार प्रेगनेंट नहीं होने के कारण सीधे किसी मेडिकल समस्या की बजाय हमारी रोजमर्रा की गलत आदतों या वातावरण से जुड़े होते हैं। इनमें प्रमुख हैं:
- अत्यधिक तनाव और चिंता: लगातार मानसिक तनाव रहने से शरीर में हार्मोन संतुलन बिगड़ सकता है, जिसका असर ओव्यूलेशन और शुक्राणु उत्पादन दोनों पर पड़ता है। शोध से पता चला है कि बांझपन की समस्या से जूझ रही महिलाओं में डिप्रेशन और ऐंग्ज़ायटी के स्तर काफी ऊंचे होते हैं। तनाव गर्भधारण को कठिन बना सकता है, इसलिए मानसिक स्वास्थ्य का ध्यान रखना आवश्यक है।
- अनियमित या असंतुलित आहार: जंक फूड, अत्यधिक कैफीन, प्रोसेस्ड फूड और पोषक तत्वों की कमी वाला खाना प्रजनन क्षमता पर नकारात्मक प्रभाव डालता है। विटामिन-डी, फॉलिक एसिड, जिंक जैसे पोषक तत्वों की कमी से हार्मोनल असंतुलन और अंडाणु/शुक्राणु की गुणवत्ता प्रभावित हो सकती है। उदाहरण के लिए, विटामिन D की कमी महिलाओं में गर्भधारण में बाधा बन सकती है।
- धूम्रपान, तंबाकू व शराब का सेवन: सिगरेट, गुटखा, शराब आदि का सेवन पुरुष और महिला दोनों में फर्टिलिटी घटाता है। निकोटीन और अल्कोहल से पुरुषों के शुक्राणु की संख्या व क्वालिटी कम हो जाती है और महिलाओं में ओवेरियन रिज़र्व घट सकता है। अनुमानतः 13-15% बांझपन के मामलों में धूम्रपान एक अहम योगदानकर्ता होता है, इसलिए इसे छोड़ना बेहतर है।
- वजन का बहुत अधिक या बहुत कम होना: अत्यधिक मोटापा (मोटापा) या अत्यंत कम वजन – दोनों ही स्थितियाँ हार्मोन असंतुलन पैदा कर सकती हैं। अधिक वजन होने से महिलाओं में PCOS, इंसुलिन रेज़िस्टेंस जैसी समस्याएँ बढ़ती हैं जो प्रजनन क्षमता घटाती हैं, वहीं बहुत दुबला होने से पीरियड्स बंद होने (एमेनोरिया) की संभावना रहती है। स्वस्थ BMI बनाए रखना गर्भधारण की संभावना के लिए लाभकारी है।
- नींद की कमी और थकान: लगातार नींद पूरी न होना भी प्रजनन स्वास्थ्य को प्रभावित कर सकता है। नींद के दौरान शरीर हार्मोन संतुलन एवं कोशिकाओं की मरम्मत करता है। यदि आप रोज़ 7-8 घंटे की अच्छी नींद नहीं लेते हैं, तो यह तनाव हार्मोन को बढ़ाकर फर्टिलिटी पर असर डाल सकता है। अतः प्रजनन आयु में महिलाओं और पुरुषों को भरपूर नींद लेने की सलाह दी जाती है।
- पर्यावरणी कारक: प्रदूषण, रासायनिक पदार्थों का संपर्क (जैसे कीटनाशक, भारी धातुएँ), प्लास्टिक में मौजूद हानिकारक पदार्थ (BPA आदि) भी धीरे-धीरे हार्मोन को प्रभावित कर सकते हैं। जिन कार्य स्थलों पर रेडिएशन, भारी धातु या विषैले कैमिकल्स हों, वहाँ काम करने वाले लोगों में बांझपन की दर सामान्य से ऊंची पाई गई है। ऐसे जोखिम कारकों से जितना हो सके बचें या उचित सुरक्षा उपाय अपनाएँ।
ऊपर बताए गए जीवनशैली कारक अक्सर धीरे-धीरे प्रभाव डालते हैं और हमें तुरंत अहसास नहीं होता। लेकिन गर्भधारण की कोशिश शुरू करने से पहले ही अगर हम अपनी आदतों को सुधार लें – जैसे स्मोकिंग छोड़ना, पौष्टिक आहार लेना, नियमित व्यायाम करना और तनाव कम करना – तो इससे प्राकृतिक रूप से फर्टिलिटी में बड़ा सुधार हो सकता है।
तनाव और भावनात्मक प्रभाव (Psychological Impact)
बांझपन की समस्या न केवल शारीरिक होती है, बल्कि इसका गहरा मनोवैज्ञानिक और भावनात्मक असर भी पड़ता है। जब महीनों/सालों प्रयास के बाद भी गर्भधारण नहीं होता, तो दंपति निराशा, दुख, कुंठा और यहाँ तक कि हीनभावना महसूस कर सकते हैं। महिलाएँ ख़ुद को दोष देने लगती हैं कि शायद उनमें ही कोई कमी है, जबकि पुरुष भी अंदर ही अंदर दुर्बल महसूस कर सकते हैं। यह तनाव पति-पत्नी के संबंधों पर दबाव डाल सकता है।
गर्भधारण में देरी से होने वाला तनाव वास्तव में एक दुष्चक्र बन सकता है – तनाव के कारण प्रेगनेंसी में और देरी होती है, और देरी के कारण फिर तनाव बढ़ता है। उच्च स्तर का स्ट्रेस हार्मोन (कॉर्टिज़ोल) महिलाओं में ओव्यूलेशन बाधित कर सकता है और पुरुषों में स्पर्म काउंट घटा सकता है। इसलिए भावनात्मक संतुलन बनाए रखना फर्टिलिटी के लिए महत्वपूर्ण है।
इस चरण में दंपति को एक-दूसरे का भावनात्मक समर्थन करना चाहिए। खुलकर बातचीत करें और एक-दूसरे की भावनाओं को समझें। यदि आवश्यक हो, तो किसी काउंसलर या थेरेपिस्ट की मदद लेने में संकोच न करें – इनफर्टिलिटी काउंसलिंग से कई कपल्स को लाभ होता है। साथ ही ध्यान, योग, प्राणायाम जैसी तनाव-नियंत्रण तकनीक अपनाने से मन शांत रहेगा और उम्मीद बंधी रहेगी। याद रखें, मानसिक रूप से सकारात्मक रहना भी आपकी उपचार प्रक्रिया का अहम हिस्सा है।
आयुर्वेदिक एवं घरेलू उपचार
बांझपन की समस्या से निपटने के लिए अनेक दंपति आधुनिक चिकित्सा के साथ-साथ पारंपरिक आयुर्वेदिक और घरेलू उपाय भी आज़माते हैं। आयुर्वेद में कुछ जड़ी-बूटियाँ और प्राकृतिक उपचार ऐसे हैं जो प्रजनन क्षमता बढ़ाने में सहायक माने जाते हैं। हालांकि इनका प्रभाव व्यक्ति-दर-व्यक्ति भिन्न हो सकता है, लेकिन संतुलित जीवनशैली के साथ ये उपाय अपनाने से संतान प्राप्ति की संभावनाएँ बेहतर हो सकती हैं:
- अश्वगंधा: अश्वगंधा को एक शक्तिशाली रसायन (टॉनिक) माना जाता है। यह तनाव कम करने, हार्मोन संतुलन और उत्तेजना बढ़ाने में मदद करती है। पुरुषों में अश्वगंधा के सेवन से शुक्राणुओं की संख्या व गतिशीलता में सुधार देखा गया है, वहीं महिलाओं में यह ओवेरियन फंक्शन को समर्थन देती है। आयुर्वेदिक चिकित्सक अक्सर बांझपन में अश्वगंधा चूर्ण या कैप्सूल लेने की सलाह देते हैं।
- शतावरी (Shatavari): शतावरी महिला प्रजनन स्वास्थ्य के लिए अत्यंत लाभकारी जड़ी-बूटी है। आयुर्वेद में इसे सदियों से स्त्री-टनिक की तरह उपयोग किया जाता है। शतावरी हार्मोन संतुलित करने, स्वस्थ ओव्यूलेशन促 करने और गर्भाशय को पोषित करने में मदद करती है। माहवारी चक्र नियमित करने और अंडाणु की गुणवत्ता सुधारने के लिए शतावरी कल्प या चूर्ण का सेवन किया जाता है।
- गोक्षुरा: गोक्षुरा (त्रिभंग) एक ऐसी जड़ी है जो पुरुष और महिला दोनों की प्रजनन क्षमता बढ़ाने में प्रयोग होती है। यह पुरुषों में टेस्टोस्टेरोन स्तर बढ़ाकर शुक्राणु वृद्धि में मदद कर सकती है, वहीं महिलाओं में भी यह हार्मोनिक बैलेंस सुधारने में सहायक है। गोक्षुरा को अक्सर अश्वगंधा-शतावरी के साथ मिलाकर औषधीय रूप में दिया जाता है।
- अन्य आयुर्वेदिक उपचार: चंद्रप्रभा वटी, पुंनर्वा, लोधरा आदि कई आयुर्वेदिक संयोजन हैं जो महिला बांझपन में उपयोग किए जाते हैं। पंचकर्म में विशेषकर उत्तर बस्ती नामक चिकित्सीय एनिमा द्वारा महिला प्रजनन अंगों की सफाई और पोषण किया जाता है, जो ट्यूब ब्लॉकेज जैसी समस्याओं में कारगर माना जाता है। इन पारंपरिक तरीकों का लाभ उठाने के लिए किसी अनुभवी आयुर्वेदाचार्य से परामर्श लें।
- घरेलू नुस्खे: कुछ घरेलू उपाय भी प्रचलित हैं, जैसे रोज़ाना एक गिलास गर्म दूध में एक चम्मच शहद मिलाकर पीना, भिगोए हुए बादाम-अखरोट का नियमित सेवन करना, या अंकुरित अनाज व मेथीदाना खाना। कहा जाता है कि इनमें विटामिन और मिनरल होते हैं जो हार्मोन संतुलन में मदद करते हैं। हालाँकि इन नुस्खों के वैज्ञानिक प्रमाण सीमित हैं, लेकिन यह सेहत के लिए नुकसानदायक नहीं हैं और समग्र स्वास्थ्य सुधार सकते हैं।
इन आयुर्वेदिक व घरेलू उपायों को आज़माते समय ध्यान रखें कि यह मुख्य चिकित्सा का विकल्प नहीं बल्कि पूरक हैं। कोई भी जड़ी-बूटी या सप्लीमेंट लेने से पहले डॉक्टर या आयुर्वेद विशेषज्ञ से सलाह अवश्य लें, खासकर यदि आप पहले से किसी चिकित्सा उपचार में हैं। प्राकृतिक उपाय धैर्य मांगते हैं – इनके साथ-साथ अपने डॉक्टर द्वारा बताए गए उपचार को जारी रखें और नियमित जांच करवाते रहें।
आहार और जीवनशैली में सुधार
गर्भधारण की समस्या को दूर करने के लिए दवा उपचार के साथ-साथ आपके आहार एवं दैनिक दिनचर्या का स्वस्थ होना भी बेहद महत्वपूर्ण है। कई बार छोटे-छोटे Diet और Lifestyle सुधार हमारी फर्टिलिटी को बड़ा बढ़ावा दे सकते हैं। निम्नलिखित उपाय अपनाकर आप अपने गर्भधारण की संभावनाएँ बढ़ा सकते हैं:
- पौष्टिक संतुलित आहार: अपने भोजन में सभी आवश्यक पोषक तत्व शामिल करें। हरी पत्तेदार सब्जियाँ, ताज़े फल, प्रोटीन (दालें, अंडा, दुबला मांस), साबुत अनाज और सूखे मेवे को आहार का हिस्सा बनाएं। फोलिक एसिड, आयरन, विटामिन-C, विटामिन-D और जिंक जैसे तत्व प्रजनन स्वास्थ्य के लिए ज़रूरी हैं। फास्ट फूड, अधिक चीनी और प्रोसेस्ड खाने से बचें। एक संतुलित आहार न केवल हार्मोन को संतुलित रखता है बल्कि शुक्राणु और अंडाणु की गुणवत्ता भी सुधारता है।
- स्वस्थ वजन बनाए रखें: जैसा ऊपर चर्चा हुआ, बहुत अधिक वजन या बेहद कम वजन – दोनों स्थितियाँ प्रजनन क्षमता के लिए ठीक नहीं। यदि आपका BMI सामान्य से ऊपर है, तो डॉक्टर की सलाह से धीरे-धीरे वजन कम करें; इससे पीरियड नियमित हो सकते हैं और ओव्यूलेशन सुधर सकता है। वहीं अति दुबले हैं तो पौष्टिक आहार से वजन बढ़ाएं ताकि शरीर गर्भधारण के लिए पर्याप्त पोषित हो। लक्ष्य एक Healthy BMI हासिल करना है, जो हार्मोन संतुलन के लिए आदर्श स्थिति प्रदान करता है।
- नियमित व्यायाम और योग: शारीरिक सक्रियता रक्त संचार बढ़ाती है और हॉर्मोन को रेग्युलेट करने में मदद करती है। रोज़ कम से कम 30 मिनट मध्यम व्यायाम (तेज़ चाल, साइकिल, तैराकी) करें। साथ ही योगासन और प्राणायाम को अपनी दिनचर्या में शामिल करें। विशेष रूप से कुछ योगासन – जैसे भद्रासन, पश्चिमोत्तानासन, सेतु बंधासन, सुप्त बद्धकोणासन – प्रजनन अंगों में रक्त प्रवाह बढ़ाकर उन्हें शक्ति देते हैं। योग से तनाव भी कम होता है, जो अप्रत्यक्ष रूप से गर्भधारण में मददगार है। ध्यान रखें बहुत अत्यधिक एक्सरसाइज (ओवर-एक्सर्शन) न करें, क्योंकि अत्यधिक शारीरिक थकान ओव्यूलेशन पर उलटा प्रभाव डाल सकती है।
- संभोग का उचित समय और आवृत्ति: गर्भधारण के लिए सही समय पर यौन संबंध बनाना महत्वपूर्ण है। महिलाओं के मासिक चक्र में जो 5-7 दिन का “फर्टाइल विंडो” (अंडोत्सर्ग के आसपास का समय) होता है, उसमें हर 1-2 दिन के अंतराल पर संबंध बनाने से गर्भधारण की संभावना बढ़ जाती है। आमतौर पर पीरियड शुरू होने के लगभग 10वें दिन से 16वें दिन तक का समय ज्यादा उपजाऊ माना जाता है, लेकिन हर महिला का चक्र अलग होता है। आप ओव्यूलेशन किट या बेसल बॉडी टेम्परेचर पद्धति से अपने ओव्यूलेशन के दिनों का पता लगा सकती हैं।
- धूम्रपान व अल्कोहल त्यागें: यदि आपने अब तक स्मोकिंग या ड्रिंक करना जारी रखा है, तो इसे तुरंत छोड़ना फर्टिलिटी सुधारने का बड़ा कदम होगा। तंबाकू और शराब दोनों ही पुरुषों और महिलाओं में फर्टिलिटी घटाते हैं (जैसा पहले उल्लेख किया गया)। इन्हें त्यागने से कुछ ही महीनों में शुक्राणु की गुणवत्ता बेहतर हो सकती है और महिलाओं में हार्मोन संतुलन सुधर सकता है।
- कैफीन और अन्य पदार्थों को सीमित करें: बहुत अधिक चाय, कॉफी (कैफीन) या कोल्ड-ड्रिंक्स लेना भी प्रजनन क्षमता पर असर डाल सकता है। दिनभर में 1-2 कप से अधिक कैफीन न लें। नशीली दवाओं या स्टेरॉयड का सेवन यदि करते हैं, तो उसे भी तुरंत बंद करें, क्योंकि ये गर्भधारण की राह में बड़ी बाधा बन सकते हैं।
- पर्याप्त नींद और आराम: रोज़ाना 7-8 घंटे की नींद लेना आपके शरीर को पुनर्जीवित करता है और हार्मोन को संतुलित रखने में मदद करता है। सोने से पहले मोबाइल/स्क्रीन को दूर रखें, अंधेरे और शांत कमरे में सोएं ताकि नींद की गुणवत्ता अच्छी हो। नींद पूरी होने से तनाव भी कम होगा और आप शारीरिक व मानसिक तौर पर स्वस्थ महसूस करेंगी।
इन आहार और जीवनशैली परिवर्तनों को अपनाने से कुछ ही महीनों में आपके शरीर में सकारात्मक परिवर्तन आने लगेंगे। याद रखें, प्राकृतिक रूप से गर्भधारण एक संपूर्ण स्वास्थ्य की मांग करता है – आपका शरीर जितना स्वस्थ और संतुलित होगा, आपके माता-पिता बनने की संभावना उतनी ही बढ़ जाएगी।
कब डॉक्टर की सलाह लें?
अगर आपने नियमित असुरक्षित संबंध बनाते हुए 12 महीने (एक वर्ष) से अधिक का समय बिता दिया है और फिर भी गर्भधारण नहीं हो पाया है, तो यह उचित समय है कि आप किसी फर्टिलिटी विशेषज्ञ/गाइनकोलॉजिस्ट से मिलें। विशेषज्ञ आम तौर पर 35 वर्ष से कम उम्र की महिलाओं को 1 वर्ष तक प्रयत्न करने की सलाह देते हैं, और 35 की उम्र के बाद 6 महीने प्रयास करने के करने के बाद डॉक्टर से संपर्क करने को कहते हैं। नीचे कुछ परिस्थितियाँ दी गई हैं जब आपको जल्द चिकित्सा सलाह लेनी चाहिए:
- एक साल प्रयास के बाद भी सफलता नहीं: यदि आप 1 वर्ष तक बिना किसी गर्भनिरोधक के नियमित प्रयास के बावजूद गर्भधारण नहीं कर पाई हैं (और आपकी आयु 35 वर्ष से कम है)। 35 से अधिक आयु होने पर 6 महीने प्रयास काफी माने जाते हैं – इसके बाद इंतज़ार किए बिना डॉक्टर को मिलें।
- पीरियड्स का असामान्य होना: यदि आपके मासिक धर्म चक्र बहुत अनियमित हैं (कभी समय पर नहीं आते या कई महीने गायब रहते हैं) या अत्यधिक दर्द और भारी रक्तस्राव वाले पीरियड्स होते हैं। अनियमित पीरियड्स ओव्यूलेशन की समस्या का संकेत हो सकते हैं, जिसका जल्द इलाज जरूरी है।
- दो या अधिक मिसकैरेज (गर्भपात): यदि आपको गर्भ ठहर तो जाता है लेकिन बार-बार प्रारंभिक महीनों में ही गर्भपात हो जाता है, तो यह प्रजनन संबंधी अंदरूनी समस्या या हार्मोन असंतुलन की ओर इशारा कर सकता है। ऐसी स्थिति में डॉक्टर व्यापक जांच करके कारण पता लगाएंगे और अगली बार गर्भ कायम रखने के लिए उपाय सुझाएंगे।
- चिकित्सा इतिहास या उम्र संबंधी कारक: अगर आपको पूर्व में पीसीओएस, एंडोमेट्रियोसिस, पेल्विक सर्जरी, यौन संक्रमण (STD) या कैंसर उपचार का इतिहास रहा है, तो गर्भ योजना शुरू करते ही डॉक्टर को अवगत कराएं। इसी तरह पुरुषों को भी अगर अतीत में टेस्टिकुलर चोट, सर्जरी या मम्प्स संक्रमण हुआ हो, तो विशेषज्ञ को बताएं। यह जानकारी डॉक्टर को सही परीक्षण चुनने में मदद करेगी।
डॉक्टर से मिलकर आप और आपके पति दोनों की संपूर्ण जांच होगी – इसमें ब्लड टेस्ट द्वारा हार्मोन लेवल चेक करना, महिलाओं के लिए अल्ट्रासाउंड/एचएसजी द्वारा गर्भाशय व ट्यूब की जांच, पुरुषों के लिए सीमेन एनालिसिस (शुक्राणु टेस्ट) शामिल है। यदि कोई वजह मिलती है तो उसका इलाज शुरू किया जाएगा। याद रखें, सही समय पर विशेषज्ञ की सलाह लेने से कीमती समय बर्बाद नहीं होगा और आप जल्दी अपने लक्ष्य की ओर बढ़ सकेंगे।
प्रेगनेंट नहीं होने का इलाज: आधुनिक उपचार विकल्प
जब प्राकृतिक प्रयास सफल न हों, तो चिकित्सा विज्ञान में आज ऐसे कई आधुनिक उपचार उपलब्ध हैं जिनकी मदद से बांझपन का समाधान किया जा सकता है। प्रेगनेंट नहीं होने का इलाज का चुनाव इस बात पर निर्भर करता है कि समस्या किस कारण से हो रही है और उसकी गम्भीरता कितनी है। डॉक्टर आपकी व आपके पार्टनर की जांच रिपोर्ट के आधार पर उचित उपचार की सलाह देंगे। आधुनिक इलाज के मुख्य विकल्प निम्न हैं:
- दवाइयों द्वारा उपचार (Ovulation Induction): महिलाओं में यदि ओव्यूलेशन संबंधी दिक्कत है तो उसका समाधान प्रायः दवाओं से किया जाता है। क्लोमीफीन साइट्रेट (Clomiphene Citrate) ऐसी ही एक दवा है जो अंडाशय को उत्तेजित कर अंडे का परिपक्व विकास促 करती है। इसके अलावा लेट्रोज़ोल व गोनाडोट्रॉपिन इंजेक्शन भी दिए जाते हैं ताकि एक चक्र में एक से अधिक अंडे विकसित हों और गर्भधारण की संभावना बढ़े। हार्मोनल असंतुलन (जैसे थायरॉयड या प्रोलैक्टिन की गड़बड़ी) होने पर डॉक्टर संबंधित हार्मोन की दवा देकर पहले उसे नियंत्रित करेंगे। पुरुषों के लिए भी कुछ दवाएं (जैसे गोनाडोट्रॉपिन या क्लोमीफीन) टेस्टोस्टेरोन बढ़ाकर शुक्राणु उत्पादन सुधारने में उपयोग होती हैं। याद रखें, ये सभी दवाएं डॉक्टर की निगरानी में ही लें।
- इंट्रायूटेरिन इन्सेमिनेशन (IUI): IUI को कृत्रिम गर्भाधान भी कहते हैं। यह उपचार तब अपनाया जाता है जब पुरुष के शुक्राणु थोड़े कमजोर या संख्या में कम हों, या महिला के गर्भाशय ग्रीवा में हल्की दिक्कत हो। IUI प्रक्रिया में पति के शुक्राणु को लैब में प्रसंस्कृत करके एक पतली ट्यूब के माध्यम से सीधे महिला के गर्भाशय में पहुंचा दिया जाता है। इसे अंडोत्सर्ग (Ovulation) के समय पर किया जाता है ताकि शुक्राणु सीधे गर्भाशय में जाकर अंडे को फर्टिलाइज़ कर सकें। IUI एक सरल व कम खर्चीला उपाय है, जिसका सहारा हल्के पुरुष बांझपन, अनइक्सप्लेंड इनफर्टिलिटी या सर्वाइकल म्यूकस की समस्या में लिया जाता है।
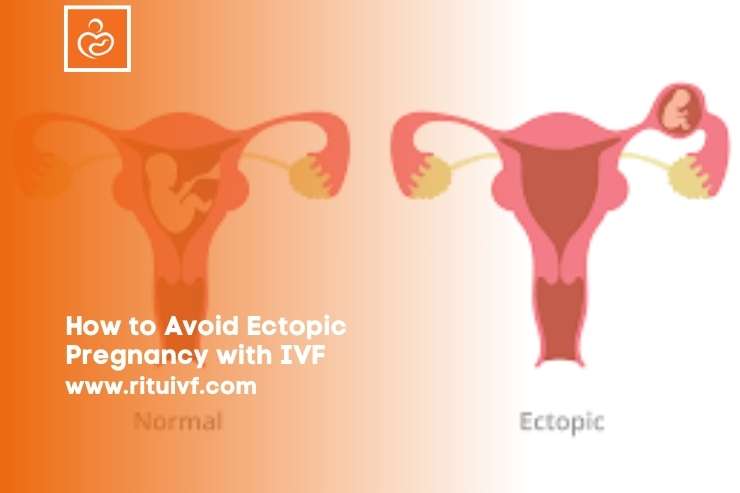
- इन-विट्रो फर्टिलाइजेशन (IVF): IVF को आम भाषा में “टेस्ट ट्यूब बेबी” तकनीक भी कहा जाता है। जब अन्य तरीकों से सफलता न मिल रही हो या कारण गंभीर हों (जैसे दोनों फैलोपियन ट्यूब ब्लॉक होना, उन्नत आयु, गंभीर पुरुष बांझपन), तब IVF अपनाया जाता है। इस प्रक्रिया में महिला के अंडाशय से अंडे निकाले जाते हैं और पुरुष के शुक्राणुओं के साथ लैब में मिलन कराया जाता है, ताकि भ्रूण बन सके। फिर 3-5 दिन बाद बने हुए भ्रूण (एंब्रियो) को महिला के गर्भाशय में स्थानांतरित कर दिया जाता है। IVF में सफलता दर उम्र और समस्या पर निर्भर करती है – युवा महिलाओं में इसकी सफलता अधिक होती है। कभी-कभी IVF चक्र के दौरान ही एक उन्नत तकनीक ICSI (Intracytoplasmic Sperm Injection) भी उपयोग की जाती है, जिसमें प्रत्येक अंडाणु के भीतर एक-एक शुक्राणु सूक्ष्म सुई द्वारा इंजेक्ट किया जाता है। ICSI सामान्यतः तब किया जाता है जब शुक्राणु संख्या या गतिशीलता बेहद कम हो।
- अन्य सहायक प्रजनन तकनीक: आधुनिक प्रजनन चिकित्सा में IVF/IUI के अतिरिक्त भी कुछ विकल्प हैं। उदाहरण के लिए, यदि महिला के अंडे पर्याप्त न बन पा रहे हों तो डोनर एग (दाता अंडाणु) का सहारा लिया जाता है जिसमें किसी अन्य स्वस्थ महिला के अंडे लेकर फर्टिलाइज किए जाते हैं और मरीज के गर्भ में रखे जाते हैं। इसी तरह गंभीर पुरुष बांझपन में डोनर स्पर्म का उपयोग किया जा सकता है। यदि महिला स्वयं भ्रूण को नौ माह धारण करने में असमर्थ हो (जैसे गर्भाशय की समस्या या लगातार गर्भपात का इतिहास), तो सरोगेसी (किसी अन्य महिला की कोख द्वारा बच्चा जन्माना) एक विकल्प होता है। इन तीसरे पक्ष की सहायता वाले विकल्पों के जरिये भी दंपति जैविक संतान पा सकते हैं, हालाँकि ये निर्णय भावनात्मक और कानूनी विचार-विमर्श के बाद ही लेने चाहिए।
- जरूरी सर्जरी: कुछ स्थितियों में सर्जरी द्वारा समस्या का समाधान किया जाता है। जैसे अगर फैलोपियन ट्यूब बंद हैं तो डॉक्टर लेप्रोस्कोपिक सर्जरी से अवरोध हटाने की कोशिश कर सकते हैं। गर्भाशय में फाइब्रॉइड या सेप्टम होने पर उन्हें हटाने के लिए हिस्टरॉस्कोपी या सर्जरी की जाती है। एंडोमेट्रियोसिस के मामले में लेप्रोस्कोपिक सर्जरी द्वारा एंडोमेट्रियल इम्प्लांट हटाए जाते हैं ताकि गर्भाशय व अंडाशय फिर सामान्य कार्य कर सकें। पुरुषों में वरीकोसील होने पर उसका ऑपरेशन (वरिकोसेलेक्टमी) किया जाता है, जिससे अक्सर शुक्राणु की गुणवत्ता में सुधार आता है। इस प्रकार, जहां आवश्यक हो, शल्य चिकित्सा बांझपन दूर करने में अहम भूमिका निभा सकती है।
उपचार का चुनाव करते समय डॉक्टर आपकी और आपके साथी की इच्छा, बजट, मेडिकल स्थिति सभी बातों को ध्यान में रखते हैं। कई मामलों में चरणबद्ध तरीके से सरल उपचार से शुरुआत कर के, आवश्यक होने पर उन्नत तकनीक तक जाया जाता है। उदाहरण के लिए, पहले कुछ महीनों दवा और IUI कराया, यदि सफल न हो तो फिर IVF की योजना बनाई। इस दौरान धैर्य रखना और डॉक्टर के निर्देशों का पालन करना जरूरी है। आधुनिक तकनीकों की बदौलत आज अधिकांश दंपतियों के लिए माता-पिता बनना संभव हो गया है, बशर्ते वे सही समय पर सही कदम उठाएं।
Ritu IVF: आपकी प्रजनन यात्रा में विश्वसनीय साथी
अगर आप लंबे समय से गर्भधारण की समस्या से जूझ रहे हैं और घर पर उपलब्ध उपायों या प्रारंभिक इलाज से लाभ नहीं हुआ है, तो एक भरोसेमंद फर्टिलिटी सेंटर का मार्गदर्शन लेना अगला उचित कदम होगा। Ritu IVF ऐसा ही एक अग्रणी आईवीएफ केंद्र है जो दंपतियों को माता-पिता बनने के सपने को साकार करने में मदद करने के लिए समर्पित है। जयपुर स्थित Ritu IVF में अत्याधुनिक प्रजनन तकनीक, वर्षों का अनुभव और करुणामयी व्यक्तिगत देखभाल का संगम मिलता है। यहां अनुभवी प्रजनन विशेषज्ञ हर मरीज के मामले को बारीकी से जाँचकर उसके हिसाब से उपचार योजना बनाते हैं। अत्याधुनिक लैब सुविधाओं और कुशल टीम के चलते Ritu IVF ने 35 वर्ष से कम आयु की महिलाओं में करीब 90% तक की सफलता दर हासिल की है, जो राष्ट्रीय औसत (लगभग 68%) से कहीं अधिक है। उच्च सफलता दर के साथ-साथ पारदर्शी मूल्य, नवीन तकनीक (जैसे लेज़र असिस्टेड हैचिंग, PGT जैसी जेनेटिक जाँच) और भावनात्मक समर्थन Ritu IVF को खास बनाते हैं। अगर आप प्रेगनेंट नहीं होने के कारण परेशान हैं, तो Ritu IVF क्लिनिक से संपर्क करके नि:शुल्क परामर्श ले सकते हैं – हो सकता है यही एक फैसला आपके जीवन में खुशियों की नई किरण लेकर आए।
अक्सर पूछे जाने वाले प्रश्न (FAQs)
प्रश्न: क्या सिर्फ महिलाओं की वजह से प्रेगनेंट नहीं होने की समस्या होती है?
उत्तर: नहीं, बांझपन के मामलों में पुरुष और महिला कारक लगभग बराबर जिम्मेदार होते हैं। आंकड़ों के अनुसार लगभग 33% मामलों में समस्या महिला पक्ष में होती है, 33% मामलों में पुरुष पक्ष में, और शेष 33% मामलों में दोनों या कारण अज्ञात होते हैं। इसलिए गर्भधारण न होने पर महिला और पुरुष दोनों की जांच करवाना महत्वपूर्ण है। कई बार पुरुष की मामूली समस्या (जैसे शुक्राणु की कमी) का हल निकालने से कपल तुरंत गर्भधारण करने में सफल हो जाते हैं।
प्रश्न: बांझपन या इनफर्टिलिटी के प्रमुख लक्षण क्या होते हैं?
उत्तर: बांझपन का मुख्य लक्षण है कि महिला गर्भवती नहीं हो पा रही है, बाकी कोई विशेष लक्षण हो भी सकते हैं या नहीं भी। कई महिलाओं में कोई स्पष्ट बाहरी लक्षण नहीं दिखते। हाँ, कुछ संकेत मिल सकते हैं जैसे बहुत अनियमित पीरियड्स या पीरियड्स का बंद हो जाना, अत्यधिक पीरियड दर्द (जो एंडोमेट्रियोसिस की ओर इशारा कर सकता है), दूध जैसा स्त्राव बिना प्रेगनेंसी (हाई प्रोलैक्टिन का संकेत) आदि। पुरुषों में भी बांझपन प्रायः बिना लक्षण के होता है, लेकिन कुछ को इrektाइल डिस्फंक्शन, स्खलन में परेशानी या अंडकोष में सूजन/दर्द जैसी दिक्कतें हो सकती हैं। यदि कोई कपल एक वर्ष तक नियमित प्रयास के बाद गर्भधारण नहीं कर पा रहा, तो यही इस बात का संकेत है कि उन्हें डॉक्टरी सलाह लेनी चाहिए।
प्रश्न: गर्भवती होने के लिए डॉक्टर को कब दिखाना चाहिए?
उत्तर: उम्र और परिस्थितियों के आधार पर ये समय अलग-अलग हो सकता है। सामान्यतः यदि पत्नी की उम्र 35 वर्ष से कम है, तो विवाह के बाद 1 साल तक कोशिश करें और गर्भधारण न हो तो फर्टिलिटी विशेषज्ञ से मिलें। 35 की उम्र के बाद 6 महीने प्रयास काफी होते हैं – उसके बाद डॉक्टर की सलाह लें। इसके अलावा यदि आपको पीरियड्स संबंधी कोई असामान्यता है, पहले से कोई गाइनेकोलॉजिकल समस्या (PCOS, फाइब्रॉइड, एंडोमेट्रियोसिस) है, या पति के सीमेन एनालिसिस में गड़बड़ी आई है – इन मामलों में बिना देर किए जल्द डॉक्टरी परामर्श लेना चाहिए। शीघ्र जांच और उपचार शुरू करने से सफलता की संभावना बढ़ जाती है।
प्रश्न: IVF क्या है और यह कब करवाना चाहिए?
उत्तर: IVF (इन विट्रो फर्टिलाइजेशन) एक प्रजनन उपचार है जिसमें महिला के अंडे और पुरुष के शुक्राणु को शरीर के बाहर प्रयोगशाला में मिलाया जाता है, फिर बने भ्रूण को महिला के गर्भाशय में प्रत्यारोपित किया जाता है। IVF उन दंपतियों के लिए सलाह दी जाती है जिनके लिए साधारण तरीके विफल हो चुके हों या जिनकी समस्या गंभीर हो – जैसे दोनों फैलोपियन ट्यूब ब्लॉक होना, उन्नत आयु (महिला की उम्र 37-40 के पार), बहुत कम शुक्राणु होना, या वर्षों से अस्पष्ट कारणों से गर्भ न ठहरना। IVF तकनीक आज काफी सफल है और लगातार इसमें सुधार हो रहा है। ज्यादातर केंद्रों में प्रति IVF चक्र 40-50% तक सफलता दर रहती है (महिला की उम्र कम हो तो और ज्यादा)। यदि डॉक्टर को लगे कि सीधे IVF से ही लाभ होगा, तो वे आपको इसके लिए सलाह देंगे। आर्थिक व मानसिक रूप से तैयार होकर ही इस प्रक्रिया को चुनें और हमेशा किसी अच्छे, विश्वसनीय IVF केंद्र का चयन करें।
प्रश्न: क्या तनाव व मानसिक स्थिति का गर्भधारण पर असर पड़ता है?
उत्तर: जी हाँ, अत्यधिक तनाव लेने से गर्भधारण कठिन हो सकता है, हालांकि हल्के-फुलके तनाव का शायद उतना प्रभाव न पड़े। लंबे समय तक डिप्रेशन या चिंता में रहने से शरीर में स्ट्रेस हार्मोन बढ़ जाते हैं जो महिलाओं में ओव्यूलेशन को दबा सकते हैं और पुरुषों में स्पर्म काउंट घटा सकते हैं। कई डॉक्टर इसीलिए बांझपन के इलाज के दौरान कपल को काउंसलिंग लेने या रिलैक्सेशन तकनीक अपनाने की सलाह देते हैं। आपको अपने मनोरंजन, योग-ध्यान, दोस्तों/परिवार का साथ इत्यादि से तनाव कम करने की कोशिश करनी चाहिए। सकारात्मक रहें – कई बार तनाव कम करते ही प्राकृतिक रूप से गर्भ ठहरने के उदाहरण भी देखने को मिले हैं। इसलिए मानसिक स्वास्थ्य को अनदेखा न करें, यह आपके संपूर्ण फर्टिलिटी ट्रीटमेंट का अहम हिस्सा है।