Have you been undergoing IUI treatment? Discover the best sleeping position after IUI to enhance implantation chances. Learn how simple adjustments can support your fertility journey for better outcomes. For instance, there are several foods you should avoid, and you also have to avoid strenuous activities. Even your sleeping position can impact the chances of your conception. So, which best position to sleep after iui is recommended by fertility specialists. Let’s find out!
Key Takeaways:
- Sleeping position plays a role in IUI success.
- Lying on your back or left side is recommended.
- Proper rest supports implantation.
The Link Between Sleeping Position & IUI Success
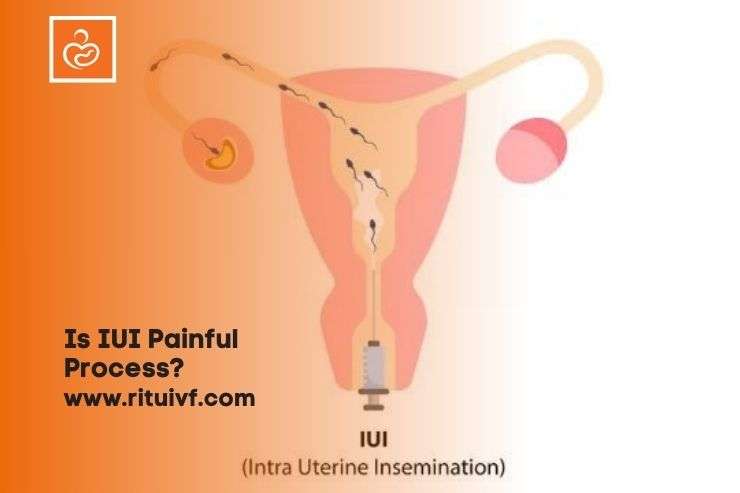
A woman’s IUI journey commences when the sperm is placed directly into the uterus with the help of a tube. Once the sperm is inside the female body, it must reach the fallopian tubes as that’s where it will encounter the waiting egg to fertilize it. The sleeping position may either hinder or aid the journey of the sperm to the fallopian tubes.
You will be amazed to learn that some sleeping positions make it easy for the sperm to get in touch with the egg. Conversely, other sleeping positions may potentially diminish the chances of conception. When you choose a proper sleeping position, you create a conducive environment and allow sperm to travel smoothly to its destination.
Best Position to Sleep After IUI
After an IUI session, rest is a must. So, today I’ll tell you everything about after IUI sleeping position.
1. Sleeping on the left side
According to doctors, an ideal sleeping position after IUI treatment is sleeping on the left side. That’s because the benefits of this sleeping position are many which include:
- an improved blood flow to the reproductive organs, thus enhancing implantation rates as well as facilitating the supply of blood to the developing embryo.
- kidney function is improved when we sleep on the left side
- relief from back pain
- good digestion
- Sleeping on your side also does not put much pressure on the vena cava which is the vein accountable for carrying blood from the body’s lower parts to the heart.
Several studies have also suggested that when a person sleeps on their left side, it encourages the movement of sperm to the mature eggs, bettering fertilization rates.
2. Sleeping with elevated hips
Right after intrauterine insemination, you should lie down comfortably on your back and keep your legs in an elevated position. Sleeping on the back is great for spinal alignment and it will also get rid of back discomfort. You can place a pillow under the hips so that they don’t hurt.
This is the best sleeping position after IUI as gravity will do its work. The sperm will go deep into the uterus and speed up the process of fertilization. If you aren’t used to sleeping in this posture, at least rest in this position for 20- 25 minutes for the sake of IUI success.
This position is best to be held immediately after your insemination. You can achieve this position by lying on your back and placing a pillow under your hips to lift them up.
This position allows gravity to do its work and ensure sperm goes deeper into your uterus and quickens fertilization. Stay in this position for 15–20 minutes after the procedure.
Explore the above-mentioned positions to find out what works for you. To promote sleep, you should practice relaxation techniques as getting fertility treatment can be extremely stressful. Staying relaxed and using supportive pillows will help you fall asleep faster.
Which Sleeping Position to Avoid After IUI
If you ask your doctor, they will always say that you should avoid sleeping on your stomach if you recently underwent IUI. The simple reason behind it is that when you lie down on your tummy, a lot of pressure is exerted on the uterus, and this can hurt your pregnancy.
Other Tips to Achieve Success with IUI
- Refrain from taking painkillers to reduce cramping after IUI.
- Do not lift heavy objects or do heavy workouts at the gym.
- Don’t skip the medications prescribed by your doctor to enhance the likelihood of conception.
- Stay away from foods that can lead to indigestion/ infection and consume nutrient-rich foods.
- Say no to smoking or drinking alcohol before, during, and after the IUI treatment.
The Bottom Line
In the end, I would like to remind you that the sleeping position alone won’t determine the success of IUI. However, it will certainly increase the chance of success.
Other than sleeping in an optimal position, you should focus on your sleep quality. Sleeping soundly at night will keep hormonal imbalances at bay, reduce stress, and strengthen your immunity. All these will positively impact your fertility levels and your pregnancy. So, make informed decisions, and soon, you will have a healthy baby playing in your arms.
Read to know: implantation bleeding after iui
FAQ’s
What is the best sleeping position after IUI?
The best sleeping position after IUI is lying on your back or left side. This helps ensure optimal blood flow to the uterus, supporting the implantation process and improving IUI success rates.
How long should I rest after IUI?
It’s recommended to rest for 15-30 minutes immediately after the IUI procedure. However, there’s no need for prolonged bed rest, and you can resume light daily activities afterward.
Can I sleep on my stomach after IUI?
Lying on your back or left side is preferred to ensure optimal blood flow to the uterus during the crucial implantation phase.
Does sleeping position affect IUI success?
Although there’s no direct evidence linking sleeping position to IUI success, lying on your back or left side can promote relaxation and support blood flow, potentially aiding implantation.
is iui a painful process?
IUI is generally not a painful process. Most women experience mild discomfort or slight cramping.
Read to know more: is iui a painful process?