The medical treatment known as intrauterine insemination (IUI) is used to treat infertility. IUI increases the likelihood of becoming pregnant by implanting specially prepared sperm directly into the uterus, the organ in which fetal development occurs. The process is also referred to as artificial insemination in certain circles.
During an IUI procedure, sperm are introduced into the uterus while an ovary releases one or more eggs. The fallopian tube, which links the uterus to the ovaries, is where it is hoped that the egg and the sperm count will eventually fuse together to form a baby. If this does occur, it will result in the chance of pregnancy.
The timing of an intrauterine pregnancy may be coordinated with a woman’s menstrual cycle. One of the two ovaries will release an egg at some point throughout the monthly cycle. Or, in conjunction with intrauterine insemination (IUI), fertility medicines may be injected to stimulate egg production in the ovaries. The specific procedure used is determined by the underlying causes of infertility.
Why was the IUI Procedure Executed?
Whether or not a couple or a person can conceive rests on many things. Most of the time, intrauterine insemination is used on women who have:
Donor Sperm: This is sperm that was given to you by someone you may or may not know. It’s a choice if you’re single, your partner doesn’t have sperm, or the sperm isn’t good enough for you to get pregnant. Intrauterine insemination is the method most often used to get pregnant for people who need to use donation sperm. Donor sperm comes from labs that have been approved, and it is thawed before the IUI process.
Unexplained Infertility: IUI is often the first treatment for people who can’t get pregnant for no clear reason. Usually, it is taken with medicines that help the ovaries make eggs.
Infertility related to endometriosis: When tissue that looks like the lining of the uterus grows outside of the uterus, it can make it hard to get pregnant. Endometriosis is the name for this. When this is the reason for infertility, the first step in treatment is often to use medicine to get a good-quality egg and do IUI.
Mild Male Factor Infertility: This is also called subfertility. Semen, the fluid that has sperm in it, can make it hard for some couples to get pregnant. A test called “semen analysis” looks at the number, size, shape, and movement of sperm to see if there are any problems. These problems are checked for by analyzing sperm. Some of these problems can be solved by IUI. This is because getting the sperm ready for the process helps separate the good ones from the bad ones.
Cervical Factor Infertility: Problems with the cervix can make it impossible to have a baby. The cervix is the thin part of the uterus at the bottom. It gives the vagina and the uterus a way to connect. During ovulation, the cervix makes mucus when the ovary releases an egg. The mucus helps the sperm move from the uterus to the fallopian tubes, where the egg is waiting. But if the mucus in the cervix is too thick, it could get in the way of the sperm. Sperm can also be stopped from getting to the egg by the cervix. The cervix can get thicker if it gets scarred, which can happen after a biopsy or other treatments. IUI skips the cervix to make it more likely that you will get pregnant. It puts the sperm right into the uterus and makes more of them ready to meet the egg.
Ovulatory Factor Infertility: IUI can also help people who can’t have children because they can’t get their eggs to mature. Some of these problems are not ovulating or not making enough eggs.
Semen Allergy: Proteins in sperm rarely cause a reaction in people who are allergic to them. When the penis sends sperm into the vagina, the area where the sperm hits the skin starts to burn and swell. A condom can keep you from getting sick, and it can also keep you from getting pregnant. IUI can make it possible to get pregnant and stop the allergy symptoms from being painful. Before the sperm is put in, many of the proteins in the sperm are taken out.
Your Level of Preparation
Before beginning the real treatment, there are a few essential tasks that must be completed, including the following:
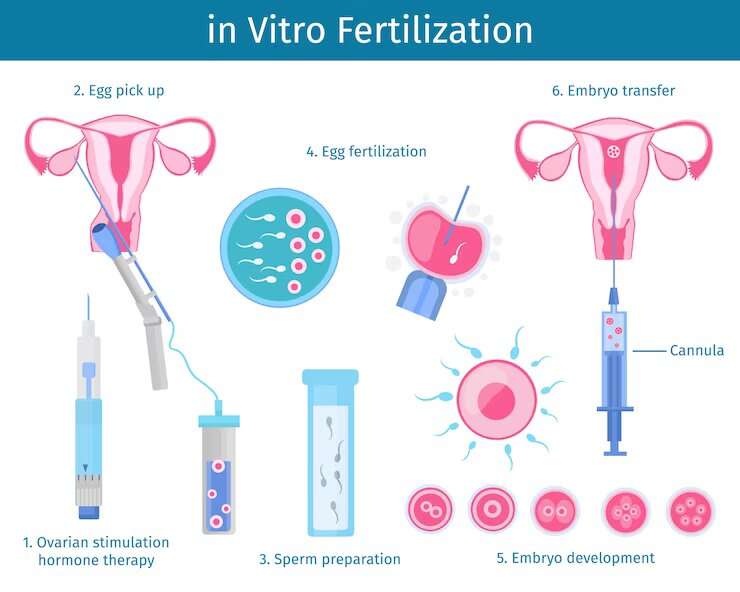
Keep an eye out for Ovulation: Because the timing of IUI is so important, it is essential to look for indicators that the body is getting ready to ovulate. You might do this by making use of a urine ovulation predictor kit that is designed for at-home usage. It is able to identify when an increase or release of luteinizing hormone (LH) occurs in your body. LH is the hormone that induces the ovary to release an egg. You might also have a procedure known as transvaginal ultrasonography, which captures pictures of your ovaries and the development of your eggs. An injection of human chorionic gonadotropin (HCG) or other medications may also be administered to you in order to induce ovulation at the optimal period. This may result in the release of one or more eggs.
Performing the surgery at the optimal time: IUI procedures are often performed one or two days after ovulation has been confirmed via diagnostic testing. Your physician will most likely have a strategy outlined for the time of your treatment as well as what to anticipate prior to the appointment.
Getting the sample of sperm ready: At the recommendation of your physician, your spouse brings in a sample of his sperm. Alternatively, one may thaw and prepare a vial containing frozen donor sperm. The sample is cleaned in such a manner that it separates the sperm that are highly active and healthy from the sperm that are of poorer quality. In addition, washing eliminates components that, if introduced into the uterus, might result in adverse responses such as severe cramping. If a small but highly concentrated quantity of healthy sperm is used, there is a greater chance of the couple getting pregnant.
During the procedure
You insert your legs into the stirrups while lying down on the exam table. The vaginal walls are opened using a speculum, a hinged instrument made of plastic or metal. Medical staff do the following throughout the procedure:
- Places a vial of viable sperm at the end of a catheter, which is a long, thin, flexible tube.
- Intravaginal catheter insertion; cervix pierced; uterus reached.
- Introduces the sperm sample into the uterus by forcing it via the tube.
- The catheter is withdrawn, then the speculum is taken out.
After the procedure.
You’ll lay on your back for a short while after the sperm has been implanted in your uterus. After the operation is over, you may go home and change into your regular clothes. After the operation, you may have some mild spotting for up to two days.
Results for Intrauterine Insemination (IUI) Treatment
Do not take a home pregnancy test for two weeks. The results of premature testing might be:
False-negative. Even if you could be pregnant, the test turns out negative. If pregnancy hormones are not yet detectable, you may obtain a false-negative test.
False-positive. The test will show a positive result for pregnancy even if you are not pregnant. Taking fertility drugs like HCG that are still in your system might cause a false-positive result.
About two weeks following the results of your at-home pregnancy test, you may be scheduled for a follow-up appointment. A blood test, which is more sensitive to the presence of pregnancy hormones after an egg has been fertilized by sperm, may be performed during the visit.
You may attempt IUI again before moving on to other fertility treatments if you don’t get pregnant the first time. In order to increase the likelihood of conception, the same medication is often administered for three to six cycles.
Conclusion:
Infertile couples might find hope and potential through IUI. Working with healthcare specialists to discover the best strategy for unique situations requires patience and persistence.







 :
:
