मातृत्व या पितृत्व का सपना हर जोड़े के लिए एक अनमोल अनुभव होता है। जब प्राकृतिक तरीके से यह सपना पूरा नहीं हो पाता, तो इन विट्रो फर्टिलाइजेशन (IVF) जैसी आधुनिक प्रजनन तकनीकें आशा की एक नई किरण लेकर आती हैं। IVF एक जटिल चिकित्सा प्रक्रिया है जिसमें अंडे और शुक्राणु को शरीर के बाहर एक प्रयोगशाला में निषेचित (फर्टिलाइज) किया जाता है, और फिर परिणामी भ्रूण को महिला के गर्भाशय में प्रत्यारोपित किया जाता है । यह बांझपन के विभिन्न कारणों, जैसे कम शुक्राणु संख्या, ओव्यूलेशन की समस्या, फैलोपियन ट्यूब में रुकावट, एंडोमेट्रियोसिस, या आनुवंशिक समस्याओं को रोकने में मदद कर सकता है। यह एकल व्यक्तियों या लैंगिक-विविध जोड़ों को भी परिवार शुरू करने में सहायता प्रदान करता है।
IVF उपचार का निर्णय लेते समय, जोड़ों के लिए सबसे महत्वपूर्ण पहलुओं में से एक इसकी लागत को समझना होता है। “जयपुर में IVF की लागत” जानना इसलिए आवश्यक है क्योंकि यह न केवल वित्तीय योजना बनाने में मदद करता है, बल्कि यह भी सुनिश्चित करता है कि आप बिना किसी अप्रत्याशित खर्च के अपने उपचार को पूरा कर सकें। IVF उपचार महंगा हो सकता है, जिसमें रक्त और इमेजिंग परीक्षण, दवाएं, अंडा निकालने और भ्रूण प्रत्यारोपण की प्रक्रियाएं, अंडे को निषेचित करने में शामिल प्रयोगशाला कार्य और भ्रूण भंडारण शामिल हैं । यह सिर्फ पैसों की बात नहीं है, यह आपके भविष्य के परिवार के सपने को साकार करने की दिशा में एक महत्वपूर्ण कदम है। यह यात्रा भावनात्मक और आर्थिक दोनों रूप से चुनौतीपूर्ण हो सकती है, और इस लेख का लक्ष्य आपको जयपुर में IVF के खर्च की पूरी जानकारी देकर पारदर्शिता के साथ मार्गदर्शन करना है।
जयपुर में IVF की लागत – एक नज़र
जयपुर में IVF की लागत कई कारकों पर निर्भर करती है, लेकिन एक बुनियादी IVF चक्र का खर्च आमतौर पर INR 1,50,000 से INR 2,50,000 के बीच होता है । हालांकि, यह ध्यान रखना महत्वपूर्ण है कि यह केवल आधारभूत लागत है और इसमें अक्सर आवश्यक दवाएं या कुछ अतिरिक्त प्रक्रियाएं शामिल नहीं होती हैं । कुछ जोड़ों को सफल गर्भाधान के लिए ₹3,00,000 से ₹4,00,000 तक का भुगतान करना पड़ा है।
IVF की लागत को प्रभावित करने वाले प्रमुख कारक (संक्षिप्त):
- क्लिनिक का प्रकार और उसकी प्रतिष्ठा
- डॉक्टर का अनुभव और उनकी योग्यता
- आवश्यक दवाओं का प्रकार और उनकी खुराक
- लैब टेक्नोलॉजी और उपयोग किए गए उपकरण
- आवश्यक IVF चक्रों की संख्या
- अतिरिक्त प्रक्रियाएं जैसे ICSI, PGT, FET की आवश्यकता
IVF का खर्च किन बातों पर निर्भर करता है?
IVF उपचार की कुल लागत कई महत्वपूर्ण कारकों से प्रभावित होती है, जिनमें से प्रत्येक का आपके वित्तीय नियोजन पर सीधा प्रभाव पड़ता है।
- क्लिनिक का अनुभव और प्रतिष्ठा: एक स्थापित और प्रतिष्ठित IVF सेंटर, जिसके पास उच्च सफलता दर और अनुभवी टीम हो, का शुल्क नए या कम अनुभवी क्लीनिकों की तुलना में अधिक हो सकता है 10। शीर्ष-स्तरीय अस्पताल, जैसे कि क्लाउडनाइन हॉस्पिटल्स, सर्वोत्तम तकनीक और बुनियादी ढांचे का उपयोग करते हैं, जो उनके शुल्क को प्रभावित करता है।
- डॉक्टर की क्वालिफिकेशन और विशेषज्ञता: अनुभवी और उच्च योग्य प्रजनन विशेषज्ञ बेहतर परिणाम सुनिश्चित करते हैं। उदाहरण के लिए, डॉ. रितु अग्रवाल जैसे विशेषज्ञ, जिनकी इस क्षेत्र में 13+ वर्षों की विशेषज्ञता है, उनकी फीस कुल लागत में योगदान करती है।
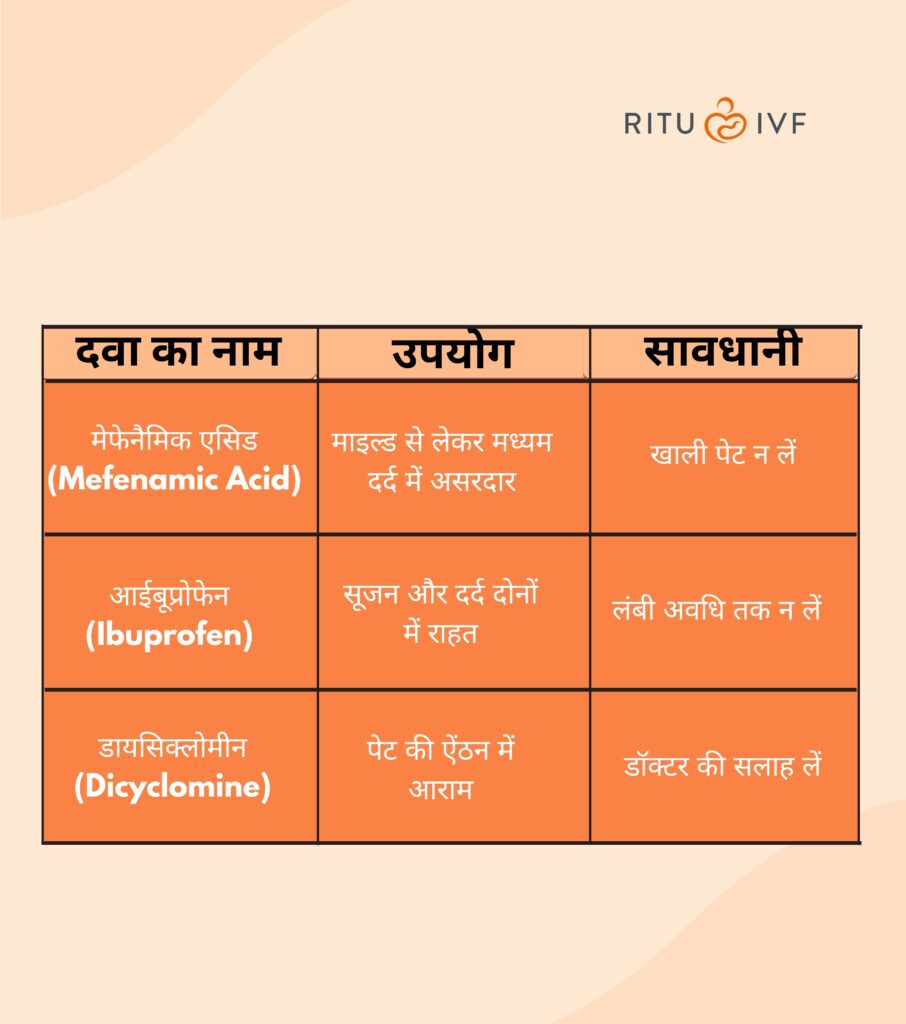
- दवाइयां और हार्मोनल इंजेक्शन: IVF प्रक्रिया में ओवेरियन स्टिमुलेशन के लिए उपयोग की जाने वाली फर्टिलिटी दवाएं और हार्मोनल इंजेक्शन (जैसे FSH, LH, HCG, प्रोजेस्टेरोन) एक महत्वपूर्ण लागत घटक होते हैं । इनकी लागत INR 20,000 से INR 70,000 या इससे भी अधिक हो सकती है, जो प्रोटोकॉल और खुराक पर निर्भर करता है 11। कुछ इंजेक्शनों की लागत ₹2,000 से ₹70,000 तक हो सकती है।
- लैब टेक्नोलॉजी और उपकरण: आधुनिक एम्ब्रियोलॉजी लैब, उन्नत उपकरण (जैसे RI Witness, AI, क्लोज्ड वर्किंग चैंबर) और कुशल एम्ब्रायोलॉजिस्ट का उपयोग उपचार की सफलता दर को बढ़ाता है, लेकिन लागत भी बढ़ाता है।
- IVF चक्रों की संख्या: सफल गर्भावस्था के लिए अक्सर एक से अधिक IVF चक्रों की आवश्यकता हो सकती है 10। प्रत्येक अतिरिक्त चक्र की लागत कुल खर्च को बढ़ा देती है, क्योंकि प्रत्येक चक्र में दवाएं और प्रक्रियाएं शामिल होती हैं।
अतिरिक्त प्रक्रियाएं और टेस्ट:
- ICSI (Intracytoplasmic Sperm Injection): यदि पुरुष बांझपन एक कारक है या शुक्राणु की गुणवत्ता कम है, तो शुक्राणु को सीधे अंडे में इंजेक्ट किया जाता है 2। यह प्रक्रिया लागत को INR 1,50,000 से INR 2,60,000 तक बढ़ा सकती है।
- PGT (Preimplantation Genetic Testing): आनुवंशिक विकारों या क्रोमोसोमल असामान्यताओं की जांच के लिए PGT की आवश्यकता हो सकती है 3। इसकी लागत INR 2,00,000 से INR 4,50,000 तक हो सकती है।
- FET (Frozen Embryo Transfer): यदि पिछले चक्र से जमे हुए भ्रूण का उपयोग किया जाता है, तो इसकी लागत INR 50,000 से INR 2,10,000 तक हो सकती है 5। इसमें भ्रूण क्रायोप्रिजर्वेशन (जमा करना) और वार्षिक भंडारण शुल्क (INR 25,000-45,000) भी शामिल है।
- डोनर अंडे/शुक्राणु/भ्रूण: यदि स्वयं के गेमेट्स का उपयोग संभव न हो, तो डोनर गेमेट्स की आवश्यकता हो सकती है, जिससे लागत में काफी वृद्धि होती है। अंडे के लिए INR 50,000-80,000 अतिरिक्त और शुक्राणु के लिए INR 8,000-12,000 अतिरिक्त लागत आ सकती है।
- अन्य टेस्ट: प्रारंभिक डायग्नोस्टिक टेस्ट, अल्ट्रासाउंड स्कैन और रक्त परीक्षण भी कुल लागत का हिस्सा होते हैं।
जयपुर में IVF की औसत लागत
यह टेबल आपको जयपुर और भारत के अन्य प्रमुख शहरों में IVF की अनुमानित लागत की तुलनात्मक जानकारी प्रदान करेगा, जिससे आपको अपने बजट और विकल्पों को समझने में मदद मिलेगी। यह रोगियों को सूचित निर्णय लेने में सहायता करता है।
जयपुर और अन्य शहरों में IVF की अनुमानित औसत लागत (एक चक्र)
| शहर |
औसत IVF लागत (INR) |
| जयपुर |
₹1,50,000 – ₹2,50,000 |
| दिल्ली |
₹1,00,000 – ₹3,00,000 |
| मुंबई |
₹1,50,000 – ₹3,00,000 |
| बेंगलुरु |
₹1,40,000 – ₹2,80,000 |
| चेन्नई |
₹1,30,000 – ₹2,70,000 |
| हैदराबाद |
₹1,20,000 – ₹2,40,000 |
| कोलकाता |
₹1,10,000 – ₹2,30,000 |
| पुणे |
₹1,20,000 – ₹2,40,000 |
नोट: ये लागतें बुनियादी IVF चक्र के लिए अनुमानित हैं और इसमें दवाएं, अतिरिक्त प्रक्रियाएं या कई चक्रों की लागत शामिल नहीं हो सकती है। लागत क्लिनिक और व्यक्तिगत आवश्यकताओं के अनुसार भिन्न हो सकती है।

IVF सफलता दर – जयपुर बनाम अन्य शहर
IVF सफलता दर एक महत्वपूर्ण विचार है, लेकिन इसे समझना जटिल हो सकता है। सफलता दर क्लिनिक, रोगी की उम्र, बांझपन का कारण और उपयोग की गई विशिष्ट तकनीकों पर बहुत निर्भर करती है ।
- जयपुर में औसत सफलता दर: जयपुर में IVF क्लीनिकों की सामान्य सफलता दर 60% से 70% तक बताई गई है । हालांकि, महिला की उम्र 35 वर्ष से कम होने पर यह दर 30% से 50% प्रति चक्र तक हो सकती है ।
- अन्य शहरों की तुलना:
- पूरे भारत में, सरकारी संस्थानों (जैसे AIIMS) में सफलता दर 30-35% से 50-60% तक हो सकती है।
- कुछ निजी क्लीनिक 70-80% तक की उच्च सफलता दर का दावा करते हैं, खासकर 35 वर्ष से कम उम्र की महिलाओं के लिए।
हैदराबाद में 35 वर्ष से कम उम्र की महिलाओं के लिए 40% सफलता दर बताई गई है।
उम्र का प्रभाव:
उम्र IVF सफलता दर का सबसे महत्वपूर्ण निर्धारक है। 35 वर्ष से कम उम्र की महिलाओं में सफलता की संभावना अधिक होती है, जबकि 40 वर्ष से अधिक उम्र की महिलाओं में यह काफी कम हो जाती है 4। 44 वर्ष की आयु तक, सफल गर्भावस्था की संभावना लगभग 1% तक गिर जाती है 21। यह दर्शाता है कि महिला की उम्र सीधे अंडे की गुणवत्ता और मात्रा को प्रभावित करती है। कम उम्र में अंडे की गुणवत्ता बेहतर होती है, जिससे भ्रूण के स्वस्थ होने और गर्भाशय में प्रत्यारोपित होने की संभावना बढ़ जाती है। जैसे-जैसे उम्र बढ़ती है, अंडे की गुणवत्ता घटती जाती है, जिससे सफल गर्भावस्था की दर कम हो जाती है और कई बार अधिक चक्रों की आवश्यकता हो सकती है, जिससे कुल लागत बढ़ जाती है। इसका मतलब है कि लागत और सफलता दर को उम्र के संदर्भ में ही देखा जाना चाहिए। यह रोगियों को यथार्थवादी अपेक्षाएं निर्धारित करने और उपचार के समय के बारे में सूचित निर्णय लेने में मदद करता है। क्लीनिकों को सफलता दरों को उम्र-समूहों में विभाजित करके प्रस्तुत करना चाहिए ताकि रोगियों को यथार्थवादी अपेक्षाएं मिल सकें। रोगियों को अपनी उम्र के आधार पर अपनी व्यक्तिगत सफलता की संभावनाओं के बारे में डॉक्टर से खुलकर बात करनी चाहिए।
IVF पैकेज और अतिरिक्त खर्च
IVF उपचार की लागत को समझने के लिए यह जानना महत्वपूर्ण है कि एक “बुनियादी पैकेज” में क्या शामिल है और कौन से खर्च अतिरिक्त हो सकते हैं।
- बुनियादी IVF पैकेज में क्या-क्या शामिल होता है? आमतौर पर, एक बुनियादी IVF पैकेज में प्रारंभिक परामर्श, कुछ डायग्नोस्टिक टेस्ट (जैसे अल्ट्रासाउंड), ओवेरियन स्टिमुलेशन (दवाओं को छोड़कर), अंडा पुनर्प्राप्ति (Egg Retrieval), शुक्राणु तैयारी (Sperm Preparation), पारंपरिक निषेचन (Conventional Fertilization), और एक ताजा भ्रूण स्थानांतरण (Fresh Embryo Transfer) शामिल होता है । कुछ क्लीनिकों में इसमें एनेस्थीसिया और निगरानी अपॉइंटमेंट भी शामिल हो सकते हैं।
- कौन-कौन से एक्स्ट्रा चार्ज लग सकते हैं? “बुनियादी पैकेज” की लागत अक्सर भ्रामक हो सकती है क्योंकि इसमें कई आवश्यक या संभावित रूप से आवश्यक प्रक्रियाएं और दवाएं शामिल नहीं होती हैं, जिससे कुल खर्च काफी बढ़ जाता है। यह रोगियों के लिए एक “छिपी हुई लागत” बन सकती है। उदाहरण के लिए, जयपुर में IVF की लागत दवाओं को छोड़कर ₹2-2.5 लाख हो सकती है । कई उन्नत प्रक्रियाएं और दवाएं अक्सर आधारभूत लागत में शामिल नहीं होती हैं । यह वित्तीय पारदर्शिता की कमी का कारण बन सकता है, जिससे रोगियों को अप्रत्याशित खर्चों का सामना करना पड़ सकता है। रोगियों को किसी भी क्लिनिक से “जयपुर में IVF पैकेज” के बारे में विस्तृत ब्रेकडाउन मांगना चाहिए, जिसमें सभी संभावित अतिरिक्त खर्चों का स्पष्ट उल्लेख हो। यह सुनिश्चित करने के लिए कि कोई अप्रत्याशित वित्तीय बोझ न पड़े, उन्हें लिखित में एक विस्तृत लागत अनुमान प्राप्त करना चाहिए। यह क्लिनिक की विश्वसनीयता को भी बढ़ाता है।
- दवाएं और इंजेक्शन: ये अक्सर अलग से बिल किए जाते हैं और कुल लागत का एक महत्वपूर्ण हिस्सा हो सकते हैं ।
- ICSI (इंट्रासाइटोप्लाज्मिक स्पर्म इंजेक्शन): पुरुष बांझपन के मामलों में आवश्यक।
- PGT/PGS (प्रीइम्प्लांटेशन जेनेटिक टेस्टिंग/स्क्रीनिंग): आनुवंशिक जांच के लिए।
- FET (फ्रोजन एम्ब्रियो ट्रांसफर): यदि ताजा भ्रूण स्थानांतरण सफल नहीं होता है या अतिरिक्त भ्रूणों का उपयोग करना हो। इसमें भ्रूण क्रायोप्रिजर्वेशन (जमा करना) और वार्षिक भंडारण शुल्क शामिल है।
- डोनर गेमेट्स (अंडे/शुक्राणु/भ्रूण): यदि स्वयं के गेमेट्स का उपयोग संभव न हो।
- सहायक हैचिंग (Assisted Hatching): भ्रूण को गर्भाशय में प्रत्यारोपित करने में मदद करने के लिए।
- एंडोमेट्रियल रिसेप्टिविटी एनालिसिस (ERA): भ्रूण स्थानांतरण के लिए सबसे अच्छा समय निर्धारित करने के लिए।
- एम्ब्रियो ग्लू (Embryo Glue): प्रत्यारोपण की संभावना बढ़ाने के लिए, खासकर कई IVF विफलताओं के बाद।
- सर्जिकल शुक्राणु पुनर्प्राप्ति (SSR/PESA/TESA): यदि शुक्राणु स्खलन में मौजूद नहीं हैं ।
IVF पैकेज में शामिल और अतिरिक्त खर्च
| घटक |
आमतौर पर बुनियादी पैकेज में शामिल |
अतिरिक्त खर्च (INR) |
| प्रारंभिक परामर्श |
हाँ |
– |
| डायग्नोस्टिक टेस्ट (शुरुआती) |
हाँ (कुछ) |
₹5,000 – ₹10,000 |
| ओवेरियन स्टिमुलेशन दवाएं |
नहीं |
₹20,000 – ₹70,000 |
| अंडा पुनर्प्राप्ति प्रक्रिया |
हाँ |
– |
| एनेस्थीसिया (पुनर्प्राप्ति के दौरान) |
हाँ (कुछ क्लीनिकों में) |
₹10,000 – ₹20,000 (यदि अलग से) |
| शुक्राणु तैयारी |
हाँ |
– |
| पारंपरिक निषेचन |
हाँ |
– |
| भ्रूण कल्चर और विकास |
हाँ |
– |
| ताजा भ्रूण स्थानांतरण |
हाँ |
– |
| ICSI (इंट्रासाइटोप्लाज्मिक स्पर्म इंजेक्शन) |
नहीं (यदि आवश्यक हो) |
₹1,50,000 – ₹2,60,000 |
| PGT (प्रीइम्प्लांटेशन जेनेटिक टेस्टिंग) |
नहीं (यदि आवश्यक हो) |
₹2,00,000 – ₹4,50,000 |
| FET (फ्रोजन एम्ब्रियो ट्रांसफर) |
नहीं (पहला FET कुछ में शामिल हो सकता है) |
₹50,000 – ₹2,10,000 |
| भ्रूण क्रायोप्रिजर्वेशन और भंडारण |
नहीं |
₹70,000 – ₹1,40,000 (क्रायोप्रिजर्वेशन), ₹25,000 – ₹45,000 (वार्षिक भंडारण) |
| डोनर अंडे |
नहीं |
₹50,000 – ₹80,000 |
| डोनर शुक्राणु |
नहीं |
₹8,000 – ₹12,000 |
| एम्ब्रियो ग्लू |
नहीं (विशेष मामलों में) |
₹5,000 – ₹10,000 |
| सर्जिकल शुक्राणु पुनर्प्राप्ति (SSR) |
नहीं (यदि आवश्यक हो) |
₹60,000 – ₹70,000 |
नोट: ये अनुमानित लागतें हैं और क्लिनिक, व्यक्तिगत आवश्यकता और उपचार प्रोटोकॉल के अनुसार भिन्न हो सकती हैं। कृपया अपने क्लिनिक से विस्तृत लागत अनुमान प्राप्त करें।
IVF में पैसे बचाने के तरीके
IVF उपचार की उच्च लागत को देखते हुए, वित्तीय बोझ को कम करने के लिए कुछ रणनीतियाँ अपनाई जा सकती हैं:
सही क्लिनिक चुनना: केवल लागत के आधार पर निर्णय नहीं लेना चाहिए। क्लिनिक की प्रतिष्ठा, सफलता दर, टीम की विशेषज्ञता और प्रदान की जाने वाली सेवाओं की पूरी श्रृंखला पर विचार करना आवश्यक है । ऐसे क्लीनिकों की तलाश करें जो पारदर्शी मूल्य निर्धारण और पैकेज प्रदान करते हैं जिसमें दवाओं की लागत शामिल हो । एक “वन-स्टॉप” क्लिनिक (जहां सोनोग्राफी, परामर्श, काउंसलिंग, हार्मोन परीक्षण, और डेकेयर सभी एक ही स्थान पर उपलब्ध हों) समय और पैसा बचा सकता है ।
पैकेज लेना और भुगतान योजनाएं: कई क्लीनिक पैकेज डील या EMI विकल्प प्रदान करते हैं, जो कुल लागत को अधिक प्रबंधनीय बना सकते हैं ।
बीमा कवरेज की जांच करें: IVF उपचार के लिए बीमा कवरेज की उपलब्धता बढ़ रही है, जो पहले दुर्लभ थी। यह रोगियों के लिए एक महत्वपूर्ण वित्तीय राहत प्रदान करता है। नए डेटा कई बीमा कंपनियों और विशिष्ट IVF बीमा उत्पादों (जैसे Safetree Fertility Insurance) को सूचीबद्ध करते हैं जो IVF उपचार को कवर करते हैं। यह एक महत्वपूर्ण उभरता हुआ रुझान है जो वित्तीय बाधाओं को कम कर सकता है। रोगियों को अपनी बीमा प्रदाता से संपर्क करना चाहिए और IVF कवरेज, प्रतीक्षा अवधि, सह-भुगतान और कटौती योग्य राशि के बारे में विस्तृत जानकारी प्राप्त करनी चाहिए। यह IVF लागत को काफी कम करने का एक प्रभावी तरीका हो सकता है।
सरकारी योजनाएं और सब्सिडी: भारत के कुछ राज्यों में, जैसे तमिलनाडु, राजस्थान, उत्तर प्रदेश, मध्य प्रदेश, बिहार और गोवा, आर्थिक रूप से कमजोर जोड़ों के लिए मुफ्त या भारी रियायती IVF उपचार उपलब्ध हैं । आयुष्मान योजना जैसी सरकारी पहलें पात्र परिवारों को रियायती IVF प्रक्रियाएं प्रदान करती हैं । राजस्थान सरकार की ART नीति भी ऐसे जोड़ों को सहायता प्रदान करती है।
अनावश्यक जांच और प्रक्रियाओं से बचें: अपने पिछले सभी टेस्ट रिपोर्ट साझा करें ताकि डॉक्टर केवल आवश्यक टेस्ट ही करवाएं । अनावश्यक भ्रूण परीक्षण (PGT) से बचना चाहिए, जब तक कि विशिष्ट संकेत न हों, क्योंकि ये महंगे होते हैं और भ्रूणों के लिए कुछ जोखिम भी पैदा करते हैं । बिना वैज्ञानिक प्रमाण वाली अतिरिक्त तकनीकों से भी बचना चाहिए।
कम क्लिनिक विज़िट: टेली-परामर्श का लाभ उठाना चाहिए जहां संभव हो, यात्रा और काम से छुट्टी के खर्च को कम करने के लिए।
Ritu IVF जयपुर में उन जोड़ों के लिए एक प्रमुख विकल्प के रूप में खड़ा है जो माता-पिता बनने के अपने सपने को साकार करना चाहते हैं। यह केंद्र कई कारणों से उत्कृष्ट है:
उच्च IVF सफलता दर (स्टैट्स के साथ): Ritu IVF 35 वर्ष से कम उम्र की महिलाओं के लिए 90% की प्रभावशाली सफलता दर का दावा करता है । यह उनकी वेबसाइट के अनुसार “राष्ट्रीय औसत 68% से कहीं अधिक” है । यह एक मजबूत दावा है, हालांकि अन्य स्वतंत्र स्रोतों द्वारा दी गई सामान्य जयपुर सफलता दर 60-70% है, और AIIMS जैसे प्रतिष्ठित संस्थान 30-35% बताते हैं। यह अंतर इस बात पर जोर देता है कि सफलता दर की व्याख्या कैसे की जाती है (जैसे, नैदानिक गर्भावस्था बनाम जीवित जन्म, प्रति चक्र बनाम संचयी, विशिष्ट आयु समूह)। क्लीनिक अक्सर अपने सबसे अनुकूल डेटा को उजागर करते हैं, जो पूरी तरह से पारदर्शी होने के बावजूद, रोगियों के लिए तुलना को जटिल बना सकता है। Ritu IVF की उच्च सफलता दर को उनके दावे के रूप में प्रस्तुत किया जाता है, साथ ही यह भी बताया जाता है कि यह 35 वर्ष से कम उम्र की महिलाओं के लिए है। यह पारदर्शिता बनाए रखता है और रोगियों को यह समझने में मदद करता है कि सफलता दर कैसे भिन्न हो सकती है।
अनुभवी डॉक्टर और एम्ब्रायोलॉजिस्ट: डॉ. रितु अग्रवाल, जयपुर की सर्वश्रेष्ठ IVF डॉक्टर, 13+ वर्षों के अनुभव के साथ, ICSI, IVF और IUI प्रक्रियाओं में विशेषज्ञ हैं। उन्होंने 18,000 से अधिक जोड़ों को माता-पिता बनने में मदद की है । उनकी विशेषज्ञता और अनुभव जटिल मामलों में भी उच्च सफलता दर सुनिश्चित करते हैं।
एडवांस लैब टेक्नोलॉजी: Ritu IVF में अत्याधुनिक तकनीक और उपकरण हैं जो अंतरराष्ट्रीय मानकों के अनुरूप हैं । उन्नत लैब तकनीकें, जैसे कि सटीक भ्रूण कल्चर और चयन, सफल परिणाम के लिए महत्वपूर्ण हैं।
पर्सनलाइज्ड केयर और ट्रांसपेरेंट कॉस्ट: IVF एक लंबी और भावनात्मक प्रक्रिया है। केवल तकनीकी दक्षता ही पर्याप्त नहीं है; रोगियों को भावनात्मक समर्थन और वित्तीय स्पष्टता की भी आवश्यकता होती है। Ritu IVF के मूल्य सीधे इन जरूरतों को पूरा करते हैं, जिससे यह सिर्फ एक चिकित्सा सुविधा से कहीं अधिक बन जाता है। क्लिनिक चुनते समय “माहौल और पर्यावरण” और “डॉक्टरों और कर्मचारियों की उपलब्धता” का महत्व व्यक्तिगत देखभाल के महत्व को दर्शाता है । इन पहलुओं को उजागर करना Ritu IVF को केवल एक क्लिनिक के रूप में नहीं, बल्कि एक सहायक भागीदार के रूप में प्रस्तुत करता है, जो भावनात्मक और वित्तीय चिंताओं को दूर करने में मदद करता है।
सैकड़ों सफल कहानियां: Ritu IVF ने 10,000 से अधिक खुशहाल रोगियों को सेवा दी है, और उनकी वेबसाइट पर सफल कहानियाँ प्रेरणा और आशा प्रदान करती हैं । यह उनके उपचार की प्रभावशीलता और रोगी संतुष्टि का प्रमाण है।
FAQs – IVF कॉस्ट से जुड़े आम सवाल
Q1: जयपुर में एक IVF चक्र की औसत लागत क्या है?
A1: जयपुर में एक बुनियादी IVF चक्र की लागत आमतौर पर ₹1,50,000 से ₹2,50,000 तक होती है, लेकिन इसमें दवाएं और अतिरिक्त प्रक्रियाएं शामिल नहीं होती हैं ।
Q2: क्या IVF उपचार बीमा द्वारा कवर किया जाता है?
A2: हाँ, अब भारत में कुछ विशिष्ट स्वास्थ्य बीमा योजनाएं IVF उपचार को कवर करती हैं। अपनी बीमा कंपनी से विवरण जानने के लिए संपर्क करें ।
Q3: IVF की लागत को प्रभावित करने वाले मुख्य कारक क्या हैं?
A3: क्लिनिक का अनुभव, डॉक्टर की योग्यता, आवश्यक दवाओं की खुराक, लैब तकनीक, और ICSI, PGT, या डोनर गेमेट्स जैसी अतिरिक्त प्रक्रियाओं की आवश्यकता मुख्य कारक हैं ।
Q4: क्या सरकारी योजनाएं IVF उपचार में मदद करती हैं?
A4: हाँ, राजस्थान सहित भारत के कुछ राज्यों में आर्थिक रूप से कमजोर जोड़ों के लिए आयुष्मान योजना और राज्य-विशिष्ट ART नीतियों के तहत मुफ्त या रियायती IVF उपचार उपलब्ध हैं ।
Q5: क्या उम्र IVF सफलता दर और लागत को प्रभावित करती है?
A5: हाँ, उम्र IVF सफलता दर का सबसे महत्वपूर्ण कारक है; कम उम्र में सफलता दर अधिक होती है। उम्र बढ़ने पर अधिक चक्रों की आवश्यकता हो सकती है, जिससे कुल लागत बढ़ सकती है ।
Q6: Ritu IVF में सफलता दर क्या है?
A6: Ritu IVF 35 वर्ष से कम उम्र की महिलाओं के लिए 90% की सफलता दर का दावा करता है ।