IVF (इन विट्रो फर्टिलाइजेशन) की प्रक्रिया कई निसंतान दंपत्तियों के लिए माता-पिता बनने की आखिरी और सबसे प्रभावी उम्मीद होती है। लेकिन जब एक या दो बार IVF साइकिल फेल हो जाती है, तो यह शारीरिक, मानसिक और आर्थिक रूप से थका देने वाला अनुभव हो सकता है।
Ritu IVF में हमारा मानना है कि “फेलियर” अंत नहीं है, बल्कि यह एक संकेत है कि हमें गहराई से जांच करने की जरूरत है। इस लेख में हम विस्तार से जानेंगे कि आखिर IVF बार-बार फेल क्यों होता है और मेडिकल साइंस में इसके क्या समाधान उपलब्ध हैं।

Trust our expert fertility team for advanced treatment, transparent care, and a proven path to parenthood.
Partner with India’s fastest-growing diagnostic network for precision testing.
IVF Success Rate: भारतीय परिप्रेक्ष्य में आंकड़े
| Age Group | 1st Cycle Success | Cumulative Success (3 cycles) | RIF के बाद Success |
|---|---|---|---|
| 25-30 वर्ष | 45-50% | 75-80% | 65-70% |
| 31-35 वर्ष | 35-40% | 65-70% | 55-60% |
| 36-39 वर्ष | 25-30% | 50-55% | 40-45% |
| 40-42 वर्ष | 15-20% | 35-40% | 25-30% |
| 43+ वर्ष | 5-10% | 15-20% | 10-15% |
IVF फेल होने का क्या मतलब है?
मेडिकल भाषा में जब तीन या उससे अधिक बार अच्छे लेवल के भ्रूण (Embryos) ट्रांसफर करने के बाद भी गर्भधारण नहीं होता, तो इसे Recurrent Implantation Failure (RIF) कहा जाता है।
IVF फेल होने के महत्वपूर्ण कारण

शुक्राणु का DNA विखंडन (Sperm DNA Fragmentation): अक्सर सारा ध्यान अंडों पर होता है, लेकिन अगर शुक्राणु के DNA में टूट-फूट (Fragmentation) अधिक है, तो भ्रूण तो बन जाएगा लेकिन वह गर्भाशय में टिक नहीं पाएगा। इसके लिए DFI (DNA Fragmentation Index) टेस्ट जरूरी है।
एंडोमेट्रियोसिस (Endometriosus): यह एक ऐसी स्थिति है जिसमें गर्भाशय के अंदरूनी ऊतक बाहर फैलने लगते हैं। यह न केवल अंडों की क्वालिटी खराब करता है, बल्कि गर्भाशय के वातावरण को भी भ्रूण के लिए “विषाक्त” (Toxic) बना सकता है।
हाइड्रोसालपिनक्स (Hydrosalpinx): यदि फेलोपियन ट्यूब में गंदा पानी भर जाए, तो वह पानी गर्भाशय में रिसकर भ्रूण को बहा सकता है या उसे इन्फेक्ट कर सकता है। ऐसी स्थिति में IVF से पहले ट्यूब को क्लिप करना या हटाना जरूरी होता है।
ब्लड क्लॉटिंग डिसऑर्डर (Thrombophilia): कुछ महिलाओं के खून में थक्के जमने की प्रवृत्ति होती है। इससे भ्रूण तक खून की सप्लाई रुक जाती है और इंप्लांटेशन फेल हो जाता है या शुरुआती गर्भपात हो जाता है।
इम्यूनोलॉजिकल फैक्टर (NK Cells): कभी-कभी महिला का शरीर भ्रूण को एक “बाहरी वस्तु” मानकर उस पर हमला कर देता है। हमारे शरीर की Natural Killer (NK) Cells अगर ज्यादा सक्रिय हों, तो वे भ्रूण को गर्भाशय में चिपकने नहीं देतीं।
मेटाबॉलिक समस्याएं (PCOS & Thyroid): अनियंत्रित थायराइड या इंसुलिन रेजिस्टेंस (PCOS) के कारण हॉर्मोन्स का संतुलन बिगड़ जाता है, जिससे भ्रूण का विकास रुक सकता है।
IVF विफलता के कारण और उनके आधुनिक समाधान (Table)
नीचे दी गई टेबल आपको समझने में मदद करेगी कि समस्या कहाँ हो सकती है और उसका समाधान क्या है:
| समस्या का क्षेत्र | मुख्य कारण | आधुनिक समाधान (Treatment) |
| अंडे/शुक्राणु | कम संख्या या खराब गुणवत्ता | Donor Egg/Sperm या ICSI तकनीक |
| भ्रूण (Embryo) | क्रोमोसोमल दोष | PGT-A / PGT-M (जेनेटिक टेस्टिंग) |
| गर्भाशय (Uterus) | पतली परत या फाइब्रॉयड्स | Hysteroscopy या PRP थेरेपी |
| इंप्लांटेशन विंडो | भ्रूण ट्रांसफर का गलत समय | ERA (Endometrial Receptivity Analysis) |
| इम्यून सिस्टम | शरीर द्वारा भ्रूण को रिजेक्ट करना | Intralipid Infusion या Immunotherapy |
IVF फेल होने के बाद क्या कदम उठाएं? (Next Steps After IVF Failure)
एक असफल साइकिल के बाद जल्दबाजी में दोबारा इलाज शुरू करने से बेहतर है कि आप थोड़ा रुकें और एक नई रणनीति तैयार करें। यहाँ स्टेप-बाय-स्टेप गाइड दी गई है:
1. विफलता का विश्लेषण (Post-Cycle Consultation)
सबसे पहले अपने फर्टिलिटी विशेषज्ञ के साथ एक विस्तृत मीटिंग करें। इसे ‘Failed Cycle Review’ कहा जाता है। अपने डॉक्टर से ये सवाल पूछें:
भ्रूण (Embryo) की क्वालिटी कैसी थी?
क्या भ्रूण के विकास में कोई समस्या आई थी?
क्या गर्भाशय की परत (Endometrium) सही मोटाई की थी?
क्या एग रिट्रीवल या ट्रांसफर के दौरान कोई तकनीकी चुनौती आई थी?
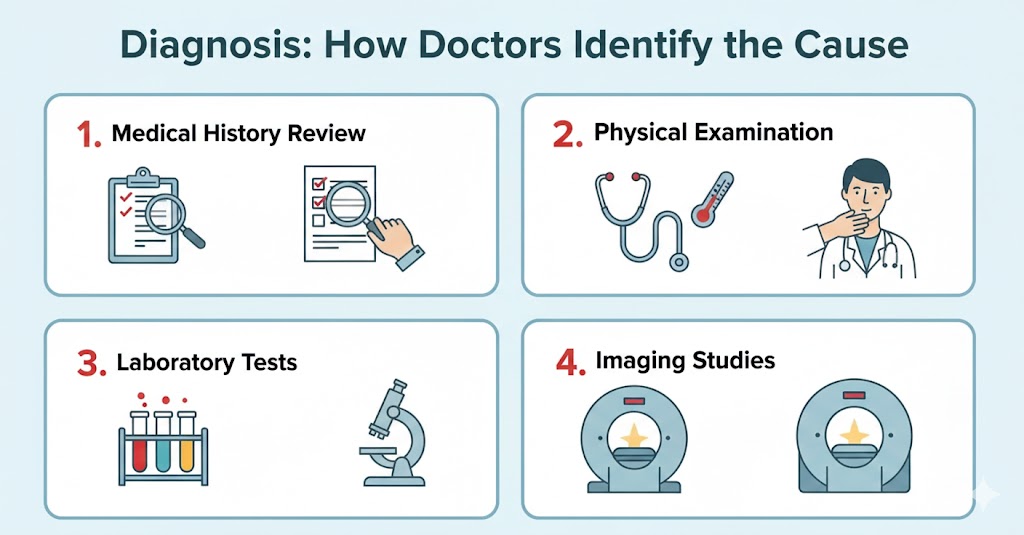
2. एडवांस डायग्नोस्टिक टेस्ट (Advanced Testing)
अगर सामान्य टेस्ट में सब ठीक था, तो अब कुछ एडवांस टेस्ट की बारी है ताकि “छिपे हुए कारणों” का पता लगाया जा सके:
ERA (Endometrial Receptivity Analysis): यह जानने के लिए कि आपका गर्भाशय भ्रूण को स्वीकार करने के लिए किस समय सबसे ज्यादा तैयार है।
PGT-A (Pre-implantation Genetic Testing): यह चेक करने के लिए कि भ्रूण जेनेटिकली सामान्य है या नहीं।
Sperm DNA Fragmentation Test: शुक्राणु के DNA की गुणवत्ता की गहराई से जांच।
3. गर्भाशय की तैयारी और हीलिंग (Uterine Healing)
कभी-कभी गर्भाशय को रिकवरी के लिए समय चाहिए होता है।
Hysteroscopy: यदि पहले नहीं की गई है, तो गर्भाशय के अंदर की किसी भी रुकावट या सूजन को देखने के लिए यह अनिवार्य है।
PRP Therapy: अगर गर्भाशय की परत (Lining) पतली है, तो एंडोमेट्रियल पीआरपी एक गेम-चेंजर साबित हो सकती है।
4. जीवनशैली और पोषण में सुधार (Lifestyle Reset)
अगली साइकिल की तैयारी कम से कम 3 महीने पहले शुरू कर देनी चाहिए:
Anti-inflammatory Diet: ओमेगा-3, एंटीऑक्सीडेंट्स और प्रोटीन युक्त आहार लें।
Weight Management: BMI को संतुलित रखने से सफलता की दर 20-30% तक बढ़ सकती है।
Supplements: डॉक्टर की सलाह पर CoQ10, फोलिक एसिड और विटामिन-D लेना शुरू करें।
5. मानसिक स्वास्थ्य और ब्रेक (Mental Health Break)
IVF का तनाव सफलता को प्रभावित कर सकता है।
खुद को दोष देना बंद करें।
योग, मेडिटेशन या किसी प्रोफेशनल काउंसलर की मदद लें।
एक या दो महीने का गैप लें ताकि आपका शरीर हॉर्मोनल इंजेक्शन के प्रभाव से बाहर आ सके।
अगली कोशिश के लिए संभावित विकल्प (Table of Options)
| स्थिति | क्या बदलाव करें? (The Shift) |
| अगर अंडे की क्वालिटी खराब है | Donor Egg या कस्टमाइज्ड हॉर्मोनल प्रोटोकॉल |
| अगर शुक्राणु में समस्या है | ICSI, IMSI या PICSI तकनीक का उपयोग |
| अगर इंप्लांटेशन नहीं हो रहा | Frozen Embryo Transfer (FET) पर विचार करें |
| अगर बार-बार गर्भपात हो रहा है | जेनेटिक स्क्रीनिंग और इम्यूनोथेरेपी |
सफलता के लिए Ritu IVF ही क्यों चुनें? (Why Choose Ritu IVF for Success?)
जब बात बार-बार IVF फेल होने की आती है, तो मरीज को एक ऐसे सेंटर की जरूरत होती है जो केवल “रूटीन इलाज” न करे, बल्कि विफलता के कारणों की गहराई तक जाए। Ritu IVF अपनी एडवांस टेक्नोलॉजी और मरीज के प्रति अपनी संवेदनशीलता के लिए जाना जाता है।
यहाँ कुछ मुख्य कारण हैं जो हमें उत्तर भारत के बेहतरीन फर्टिलिटी सेंटर्स में से एक बनाते हैं:
1. एडवांस लैब और आधुनिक टेक्नोलॉजी (State-of-the-art Lab)
IVF की सफलता का 70% श्रेय लैब की गुणवत्ता को जाता है। Ritu IVF में हमारे पास विश्व स्तरीय Class-100 IVF Lab है, जहाँ भ्रूण को बिल्कुल माँ के गर्भ जैसा वातावरण मिलता है। हम ICSI, IMSI, और Laser-Assisted Hatching जैसी आधुनिक तकनीकों का उपयोग करते हैं जो फेलियर के मामलों में सफलता दर को बढ़ा देती हैं।
2. अनुभवी विशेषज्ञों की टीम (Expert Specialists)
हमारे पास अनुभवी फर्टिलिटी विशेषज्ञों और भ्रूण वैज्ञानिकों (Embryologists) की एक टीम है, जिन्होंने हजारों सफल केस हैंडल किए हैं। बार-बार फेल हुए जटिल मामलों को सुलझाना हमारी विशेषज्ञता है।
3. पर्सनलाइज्ड ट्रीटमेंट प्लान (Individualized Care)
हम “One Size Fits All” के सिद्धांत पर विश्वास नहीं करते। हर कपल की मेडिकल हिस्ट्री अलग होती है। हम विफलता के कारणों (जैसे पतली एंडोमेट्रियम, DNA फ्रेगमेंटेशन या जेनेटिक इश्यूज) की पहचान करते हैं और फिर एक कस्टमाइज्ड प्रोटोकॉल तैयार करते हैं।
4. उच्च सफलता दर (High Success Rate)
Ritu IVF ने उन कपल्स को भी खुशियां दी हैं जिन्होंने 3-4 बार अन्य जगहों पर विफलता का सामना किया था। हमारी Frozen Embryo Transfer (FET) और Blastocyst (Day 5) Transfer की तकनीक सफलता की संभावना को 60-70% तक ले जाती है।
5. पारदर्शी और किफायती इलाज (Transparency & Affordability)
हम इलाज की प्रक्रिया और खर्चों को लेकर पूरी पारदर्शिता रखते हैं। कोई छिपे हुए शुल्क (Hidden Charges) नहीं होते। हमारा उद्देश्य कम से कम खर्च में बेहतरीन मेडिकल सुविधाएं प्रदान करना है।
6. मनोवैज्ञानिक और भावनात्मक सहयोग (Compassionate Counseling)
हम समझते हैं कि IVF फेल होने के बाद एक कपल किस दौर से गुजरता है। इसलिए, हम चिकित्सा के साथ-साथ भावनात्मक काउंसलिंग भी प्रदान करते हैं, ताकि आप मानसिक रूप से मजबूत होकर अपनी अगली सफल यात्रा शुरू कर सकें।
Ritu IVF की विशेष सेवाएं जो सफलता सुनिश्चित करती हैं:
ERA (Endometrial Receptivity Analysis): इंप्लांटेशन का सही समय जानने के लिए।
PGT (Pre-implantation Genetic Testing): केवल स्वस्थ और अनुवांशिक रूप से सही भ्रूण का चयन।
Advanced Male Infertility Clinic: शुक्राणु संबंधी गंभीर समस्याओं का इलाज।
Donor Program: हाई-क्वालिटी डोनर एग और स्पर्म बैंक की सुविधा।
अक्सर पूछे जाने वाले प्रश्न (FAQs) – Ritu IVF Special
Q1. कितनी बार IVF फेल होने के बाद उम्मीद छोड़ देनी चाहिए?
उत्तर: चिकित्सा विज्ञान में ‘हार मानने’ जैसी कोई निश्चित संख्या नहीं है। आमतौर पर 3-4 असफल प्रयासों के बाद विस्तृत जांच (Detailed Investigation) की आवश्यकता होती है। कई दंपत्ति सही एडवांस तकनीक और डॉक्टर के मार्गदर्शन से 5वीं या 6वीं साइकिल में भी सफल होते हैं। यह आपकी आयु, मेडिकल स्थिति और भावनात्मक शक्ति पर निर्भर करता है।
Q2. क्या IVF फेल होने के बाद नेचुरल प्रेगनेंसी (Natural Pregnancy) संभव है?
उत्तर: हाँ, यह संभव है। विशेषकर उन मामलों में जहाँ बांझपन का कारण “Unexplained Infertility” (अस्पष्ट बांझपन) हो। कभी-कभी IVF के दौरान इस्तेमाल की गई दवाएं और हॉर्मोनल सुधार शरीर के नेचुरल सिस्टम को एक्टिव कर देते हैं, जिससे फेलियर के बाद प्राकृतिक गर्भधारण की संभावना बन सकती है।
Q3. IVF फेल होने के मुख्य लक्षण (Symptoms) क्या हैं?
उत्तर: IVF फेल होने का सबसे स्पष्ट लक्षण ‘बीटा एचसीजी’ (Beta-HCG) ब्लड टेस्ट का नेगेटिव आना या एम्ब्रयो ट्रांसफर के 14 दिनों बाद पीरियड्स का शुरू होना है। कुछ महिलाओं को हल्का स्पॉटिंग या क्रैम्प्स महसूस हो सकते हैं, लेकिन बिना मेडिकल टेस्ट के विफलता की पुष्टि नहीं की जा सकती।
Q4. ERA टेस्ट क्या है और यह कब करवाना चाहिए?
उत्तर: ERA (Endometrial Receptivity Analysis) एक एडवांस टेस्ट है जो गर्भाशय की परत की जांच करता है। यदि आपके 2-3 बार अच्छी गुणवत्ता वाले भ्रूण (High-quality embryos) ट्रांसफर करने के बाद भी प्रेगनेंसी नहीं हुई है, तो यह टेस्ट यह बताता है कि भ्रूण ट्रांसफर करने का सबसे सही समय (Implantation Window) कौन सा है।
Q5. क्या तनाव (Stress) सच में IVF विफलता का कारण बनता है?
उत्तर: तनाव सीधे तौर पर IVF फेल नहीं करता, लेकिन अत्यधिक और लंबे समय तक बना रहने वाला तनाव शरीर में कोर्टिसोल और अन्य हॉर्मोन्स का संतुलन बिगाड़ देता है। इससे गर्भाशय में रक्त का प्रवाह प्रभावित हो सकता है, जो इंप्लांटेशन के लिए बाधा बन सकता है। इसलिए रिलैक्सेशन तकनीकों की सलाह दी जाती है।
Q6. अगली IVF साइकिल शुरू करने से पहले कितना गैप (Break) लेना चाहिए?
उत्तर: शारीरिक और मानसिक रिकवरी के लिए कम से कम 2 से 3 महीने (यानी 2-3 पीरियड्स साइकिल) का गैप लेना सबसे अच्छा माना जाता है। इस समय का उपयोग खान-पान सुधारने, वजन संतुलित करने और जरूरी एडवांस टेस्ट करवाने में करना चाहिए।